En español | You probably know someone who’s traded a worn-out hip bone for ceramic or cobalt chrome. Some 370,000 Americans undergo hip-replacement surgery each year (the average age for this is 65). But the operation isn’t a cure-all: At least 1 in 10 hip-replacement recipients will need a second procedure to repair a dislocation, mechanical failure or infection. And hip pain, with or without surgery, can be a struggle. Chronic hip pain was a factor in the accidental opioid overdoses that claimed the lives of musicians Tom Petty, 66, and Prince, 57.
Your hip labrum is a band of cartilage-like tissue that courses around the outer rim of your hip socket. This labrum helps to support the joint and deepen the socket. Sometimes overuse or an injury to your hip can cause a tear in your labrum. A hip labrum tear may result in a condition called femoroacetabular impingement (FAI). When this happens, hip pain may result, and exercises to stretch and stabilize your hip may be performed. 
Paget's disease can be diagnosed on plain X-rays. However, a bone biopsy is occasionally necessary to ensure the accuracy of the diagnosis. Bone scanning is helpful to determine the extent of the disease, which can involve more than one bone area. A blood test, alkaline phosphatase, is useful for diagnosis andmonitoring response to therapy. Treatment options include aspirin, other anti-inflammatory medicines, pain medications, and medications that slow therate of bone turnover, such as calcitonin (Calcimar, Miacalcin), etidronate (Didronel), alendronate (Fosamax), risedronate (Actonel), and pamidronate (Aredia).
When was the last time you got on your gym's abductor or adductor machine and got in a good workout? It's probably been a while. Both are machines that don't get a lot of use, and they are often the target of coaches' ridicule on those "useless gym moves we should all skip" lists. Perhaps rightly so, especially if you're hopping on those machines hoping for a slimming effect.
Lay on your back on your mat and pull your knees to your chest. Place your hands on the inside arches of your feet and open your knees wider than shoulder-width apart. Keeping your back pressed into the mat as much as possible, press your feet into hands while pulling down on feet, creating resistance. Breathe deeply and hold for at least 30 seconds.

If you have arthritis or bursitis, you’ve probably noticed that exercise can actually help relieve your pain. But when is hip pain a sign that you should stop exercising or doing a certain activity? If your hip starts to hurt during a particular exercise and lingers for hours or days afterward, that’s a sign that your joint needs to rest, notes Humphrey. It’s normal to feel some soreness the day after exercising, but the pain shouldn’t persist or become worse. Also, if you experience a sharp or shooting pain, stop the activity immediately and talk to your doctor or physical therapist.
Radicular pain. This type of pain can occur if a spinal nerve root becomes impinged or inflamed. Radicular pain may follow a nerve root pattern or dermatome down into the buttock and/or leg. Its specific sensation is sharp, electric, burning-type pain and can be associated with numbness or weakness (sciatica). It is typically felt on only one side of the body.
Congenital bone conditions: Congenital causes (existing from birth) of low back pain include scoliosis and spina bifida. Scoliosis is a sideways (lateral) curvature of the spine that can be caused when one lower extremity is shorter than the other (functional scoliosis) or because of an abnormal architecture of the spine (structural scoliosis). Children who are significantly affected by structural scoliosis may require treatment with bracing and/or surgery to the spine. Adults infrequently are treated surgically but often benefit by support bracing. Spina bifida is a birth defect in the bony vertebral arch over the spinal canal, often with absence of the spinous process. This birth defect most commonly affects the lowest lumbar vertebra and the top of the sacrum. Occasionally, there are abnormal tufts of hair on the skin of the involved area. Spina bifida can be a minor bony abnormality without symptoms. However, the condition can also be accompanied by serious nervous abnormalities of the lower extremities.
The story of actor Andy Whitfield is a disturbing and educational example of a case that met these conditions — for sure the first two, and probably the third as well if we knew the details. Whitfield was the star of the hit TV show Spartacus (which is worthwhile, but rated very, very R17). The first sign of the cancer that killed him in 2011 was steadily worsening back pain. It’s always hard to diagnose a cancer that starts this way, but Whitfield was in the middle of intense physical training to look the part of history’s most famous gladiator. Back pain didn’t seem unusual at first, and some other symptoms may have been obscured. Weight loss could have even seemed like a training victory at first! It was many long months before he was diagnosed — not until the back pain was severe and constant. A scan finally revealed a large tumour pressing against his spine.

Really a great content. Let me tell you first about hip flexor it is the engine through which our body moves. They control balance, our ability to sit, stand, twist, reach, bend, walk and step. One of my patient also suffering from same problem but due to lack of money he was unable to afford a treatment. So i recommend him a program to unlock hip flexor. If anyone wants they can check it out here ;- https://tinyurl.com/y8yaqs2s Report
Six sciatica stretches for pain relief Sciatica is nerve pain that runs through the buttocks, down the back of the leg and into the ankle or foot. It is a symptom of several different back, pelvis, and hip problems, and can also occur as a result of pregnancy. Stretching can provide relief from the pain. Here, we suggest six stretches to perform every day. Read now
You'll need a resistance band for this one. With this exercise you're focusing on four movements—flexion, extension, abduction and adduction. Try and stand up straight while doing the exercise. If you have to lean excessively, step closer to the anchor point of your band to decrease resistance. You'll find that not only are you working the muscles of the leg that's moving, the muscles of your stance leg will work quite hard stabilizing and balancing.
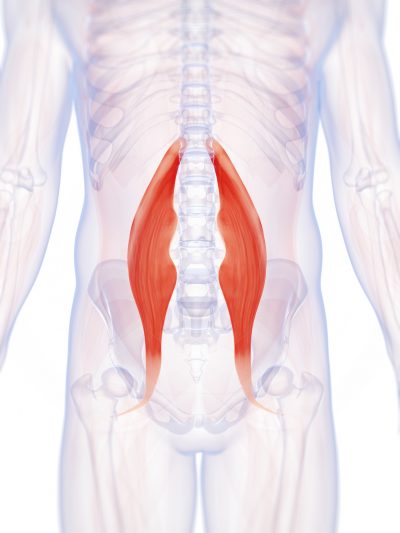
Located deep in the front of the hip and connecting the leg, pelvis, and abdomen, the hip flexors— surprise, surprise— flex the hip. But despite being some of the most powerful muscles in our bodies (with a clearly important role), it’s easy to neglect our poor hip flexors— often without even knowing it. It turns out just working at a desk all day (guilty!) can really weaken hip flexors since they tend to shorten up while in a seated position. This tightness disrupts good posture and is a common cause of lower back pain. Weakened hip flexors can also increase the risk of foot, ankle, and knee injuries (especially among runners) Hip muscle weakness and overuse injuries in recreational runners. Niemuth, P.E., Johnson, R.J., Myers, M.J., et al. Rocky Mountain University of Health Professions, Provo, VT. Clinical Journal of Sport Medicine, 2005 Jan; 15 (1): 14-21.. So be sure to get up, stand up every hour or so! And giving the hip flexors some extra attention is not just about injury prevention. Adding power to workouts, working toward greater flexibility, and getting speedier while running is also, as they say, all in the hips The effect of walking speed on muscle function and mechanical energetics. Neptune, R.R., Sasaki, K., and Kautz, S.A. Department of Mechanical Engineering, The University of Texas, Austin, TX. Gait & Posture, 2008 Jul; 28 (1): 135-43..

Sit on floor with knees bent and shins stacked with right leg on top. Use your hand to position right ankle on left knee. Ideally, the right knee will rest on the left thigh, but if your hips are tight, your right knee may point up toward the ceiling (overtime, as your hips become more open, your knee will lower). Keeping your hips squared to the front of the room, hinge at the hips and slowly walk hands slightly forward. If this is enough of a stretch, hold here, or fold your torso over your thighs to go deeper. Hold for at least 30 seconds, then repeat on opposite side.
Degenerative bone and joint conditions: As we age, the water and protein content of the body's cartilage changes. This change results in weaker, thinner, and more fragile cartilage. Because both the discs and the joints that stack the vertebrae (facet joints) are partly composed of cartilage, these areas are subject to wear and tear over time (degenerative changes). Degeneration of the disc is called spondylosis. Spondylosis can be noted on X-rays of the spine as a narrowing of the normal "disc space" between the vertebrae. It is the deterioration of the disc tissue that predisposes the disc to herniation and localized lumbar pain ("lumbago") in older patients. Degenerative arthritis (osteoarthritis) of the facet joints is also a cause of localized lumbar pain that can be detected with plain X-ray testing. These causes of degenerative back pain are usually treated conservatively with intermittent heat, rest, rehabilitative exercises, and medications to relieve pain, muscle spasm, and inflammation.
According to a study published in Annals of Internal Medicine, there is strong evidence that yoga can have a short-term effect on treating lower back pain. Yoga involves slow, controlled movements to stretch and strengthen the body. This exercise form also promotes stress relief, which can help reduce tension you may commonly hold in your lower back.
Iliopsoas syndrome, which is also called psoas syndrome or iliopsoas tendonitis, occurs when the iliopsoas muscles are injured. Lower back pain is the most common symptom; however, pain can also occur in the hip, thigh, or leg. The iliopsoas bursa, which is a fluid-filled sac located on the inside of the hip that reduces rubbing and friction, is also likely to become inflamed due to the proximity of the two structures. When this happens, the inflamed bursae will make it difficult to move.

The hip joint is designed to withstand a fair amount of wear and tear, but it’s not indestructible. For example, when you walk, a cushion of cartilage helps prevent friction as the hip bone moves in its socket. With age and use, this cartilage can wear down or become damaged, or the hip bone itself can be fractured during a fall. In fact, more than 300,000 adults over 65 are hospitalized for hip fractures each year, according to the Agency for Healthcare Research and Quality.

Running: Running may be good for boosting your cardiovascular health but it can be very strenuous if you have hip pain. The impact can upset your hip joints so instead focus on other forms of exercise. Walking is still a good option for hip pain if you really feel like working out in the great outdoors or you could instead try some strengthening exercises from the comfort of your own home.
How to: Sit on the floor with knees bent so that your right shin is positioned in front of you, your left shin behind you and your left hip dropped all of the way to the floor (a). Inhale and press your left hip forward until you feel a stretch in the front of your hip (b). Exhale and press left hip back to the floor. That’s one rep (c). Complete six to eight reps, working each time to increase your range of motion. Repeat on the opposite side.
There are many causes of hip joint pain. Some hip pain is temporary, while other hip pain can be long-standing or chronic. Causes of hip pain include arthritis, inflammatory and noninflammatory arthritis, fracture, sprain, infectious arthritis (septic arthritis), avascular necrosis, Gaucher's disease, sciatica, muscle strain, iliotibial band syndrome (IT band syndrome), and hematoma.
I think you should mention that for some people, stretching is not the solution and that it will deteriorate their posture. Some people need stretching, but most people I know need to strengthen their "overstretched" hip flexors. Many people can't do a single hanging leg raise. Check this site if you want to know more about the importance of hip flexors bit.ly/Unlock_Your_Hip_Flexor Report

Hamstring squeeze. Use the machine that works your hamstrings; you will either lie on your stomach or sit with a pad behind your knee. Push against the pad, moving your knee up toward the ceiling or backward (depending on which position you’re in). “In other words, bend your knees,” Pariser says. But to avoid cramps in your hamstring muscles, don’t bend your knee so much that your heels are too close to your buttocks.
I think you should mention that for some people, stretching is not the solution and that it will deteriorate their posture. Some people need stretching, but most people I know need to strengthen their "overstretched" hip flexors. Many people can't do a single hanging leg raise. Check this site if you want to know more about the importance of hip flexors bit.ly/Unlock_Your_Hip_Flexor Report
You can strain or tear one or more of your hip flexors when you make sudden movements such as changing directions while running or kicking. Sports and athletic activities where this is likely to occur include running, football, soccer, martial arts, dancing, and hockey. In everyday life, you can strain a hip flexor when you slip and fall, for example.
I’m a runner and started experiencing some familiar tightness in my hip and started getting worse everyday I ran. It’s always gotten sore after running for a long extent for the last 4 years or so. I’m glad I found this page because all of these stretches helped me realize what needed to be stretched and how tight I really was! I hope this will fix my overwhelming soreness. Thank you!

A traumatic injury, such as from playing sports, car accidents, or a fall can injure tendons, ligaments or muscle resulting in low back pain. Traumatic injury may also cause the spine to become overly compressed, which in turn can cause an intervertebral disc to rupture or herniate, exerting pressure on any of the nerves rooted to the spinal cord. When spinal nerves become compressed and irritated, back pain and sciatica may result.
Veritas Health publishes original and accessible health related content written by more than 100 physician authors and peer-reviewed by a 16 member Medical Advisory Board. The Veritas Health platform comprising of Spine-health.com, Arthritis-health.com, Sports-health.com, and Pain-health.com, provides comprehensive information on back pain, arthritis, sports injuries, and chronic pain conditions. For more information visit Veritashealth.com.

THIS TOOL DOES NOT PROVIDE MEDICAL ADVICE. It is intended for general informational purposes only and does not address individual circumstances. It is not a substitute for professional medical advice, diagnosis or treatment and should not be relied on to make decisions about your health. Never ignore professional medical advice in seeking treatment because of something you have read on the WebMD Site. If you think you may have a medical emergency, immediately call your doctor or dial 911.
Neglect your lower body too often and you risk losing mobility — that thing that allows you to plop down on the floor to play with your kids, or get up and out of even the cushiest chair with ease. “A lot of people sit all day, so they’re not necessarily using their glute muscles,” says Daily Burn Fitness/Nutrition Coach Allie Whitesides. “And a lot of people are in the car all the time, so we’re not using our leg muscles much, either.”

Luckily, you don’t have to quit your day job or forgo spin class to loosen them up. Simply stretching those hips can get your body back in alignment, increase your mobility (and thus your exercise performance) and maybe even ease pesky back pain, Moore says. “Given the amount of time we sit [each] day and the stress we put our bodies under, hip-opening moves are a necessary party of our daily routine.”
Medicine FinderLatest NewsSlip, slap, slop early to save your skinComplementary medicine users have worse cancer survivalVideo: BoredomPut down the tablet; pick up a bookVideo: Lift your mood with some weightsQuicken your step to live longerThis web site is intended for Australian residents and is not a substitute for independent professional advice. Information and interactions contained in this Web site are for information purposes only and are not intended to be used to diagnose, treat, cure or prevent any disease. Further, the accuracy, currency and completeness of the information available on this Web site cannot be guaranteed. Tonic Digital Media Pty Ltd, its affiliates and their respective servants and agents do not accept any liability for any injury, loss or damage incurred by use of or reliance on the information made available via or through myDr whether arising from negligence or otherwise. See Privacy Policy and Disclaimer.2001-2019 myDr.com.au © | All Rights Reserved About UsContact UsDisclaimerPrivacy PolicyAdvertising PolicySitemap
Medications: A wide range of medications are used to treat acute and chronic low back pain. Some are available over the counter (OTC); others require a physician’s prescription. Certain drugs, even those available OTC, may be unsafe during pregnancy, may interact with other medications, cause side effects, or lead to serious adverse effects such as liver damage or gastrointestinal ulcers and bleeding. Consultation with a health care provider is advised before use. The following are the main types of medications used for low back pain:
The hip flexors play an important role in everyday mobility and exercise. Involved in pulling the knee toward the hip, most movements either directly or indirectly use the hip flexors. That’s why even the slightest injury can cause great discomfort. Learn how you can recover from a hip flexor injury, and what precautions can be taken to avoid them.