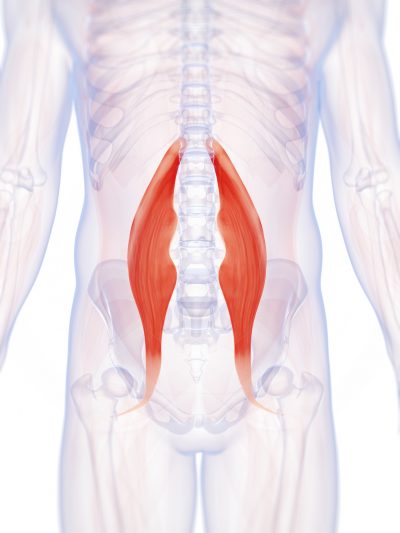
Lumbar strain (acute, chronic): A lumbar strain is a stretch injury to the ligaments, tendons, and/or muscles of the low back. The stretching incident results in microscopic tears of varying degrees in these tissues. Lumbar strain is considered one of the most common causes of low back pain. The injury can occur because of overuse, improper use, or trauma. Soft-tissue injury is commonly classified as "acute" if it has been present for days to weeks. If the strain lasts longer than three months, it is referred to as "chronic." Lumbar strain most often occurs in people in their 40s, but it can happen at any age. The condition is characterized by localized discomfort in the low back area with onset after an event that mechanically stressed the lumbar tissues. The severity of the injury ranges from mild to severe, depending on the degree of strain and resulting spasm of the muscles of the low back. The diagnosis of lumbar strain is based on the history of injury, the location of the pain, and exclusion of nervous system injury. Usually, X-ray testing is only helpful to exclude bone abnormalities.
However, even the things you do every day — like sitting in front of a computer or at a desk for hours — can both weaken and shorten (tighten) your hip flexors, making them more prone to injury. Because of this, exercises (such as squats) and targeted stretches which focus on strengthening the hip muscles and improving hip mobility are key to preventing injuries.
Honestly, I am new to a lot of this stuff, so I am definitely not an expert on the subject. However, I have been doing some research on the matter, and it seems most people recommend stretching the opposing muscle group in such cases. For example, if you injured your hamstring, you would stretch your thigh. You would also want to stretch the surrounding muscle groups, seeing as how our entire body is fit together, so that every part of your body affects every other part. I realize that by now you are probably back to skating, but for anyone else who reads this and has a similar issue, I would still suggest looking into it a bit, as, like I said, I am new to a lot of stuff (PE was about as far as I got when it came to exercise, until almost two months ago, when I found crossfit), but at least it’s a start.
The condition is cauda equina syndrome. It involves “acute loss of function of the neurologic elements (nerve roots) of the spinal canal below the termination (conus) of the spinal cord,” where the nerves spread out like a horse (equina) tail. Again, this condition causes symptoms in the “saddle” of the body: butt, groin, inner thighs. BACK TO TEXT
Icing a joint that’s inflamed because of arthritis or bursitis can lower inflammation and help with hip pain. “If it’s very painful, I sometimes tell patients to ice four or five times daily for about 10 to 15 minutes,” says Amy Humphrey, DPT, a physical therapist at Body Dynamics, Inc. in Arlington, Va. Use an ice pack, wrap a towel around it, and put it where you feel the pain.

Bony encroachment: Any condition that results in movement or growth of the vertebrae of the lumbar spine can limit the space (encroachment) for the adjacent spinal cord and nerves. Causes of bony encroachment of the spinal nerves include foraminal narrowing (narrowing of the portal through which the spinal nerve passes from the spinal column, out of the spinal canal to the body, commonly as a result of arthritis), spondylolisthesis (slippage of one vertebra relative to another), and spinal stenosis (compression of the nerve roots or spinal cord by bony spurs or other soft tissues in the spinal canal). Spinal-nerve compression in these conditions can lead to sciatica pain that radiates down the lower extremities. Spinal stenosis can cause lower-extremity pains that worsen with walking and are relieved by resting (mimicking the pains of poor circulation). Treatment of these afflictions varies, depending on their severity, and ranges from rest and exercises to epidural cortisone injections and surgical decompression by removing the bone that is compressing the nervous tissue.
This standard recommendation reinforces the alarming idea that low back pain that lasts longer than a few weeks is Really Bad News. It’s not. It’s a clue. It’s a reason for concern and alertness. But many cases of low back pain that last for 6 weeks will still go away. Once again, see the 2009 research published in the British Medical Journal, which showed that more than 30% of patients with “new” chronic low back pain will still recover without treatment. BACK TO TEXT
Place a mini band around your ankles and spread your feet about shoulder-width apart. Keeping your legs relatively straight (you want the motion to come from your hips) and toes pointing forward, walk forward 10 steps, then backward 10 steps. Take a short break and then walk to the right 10 steps, then to the left 10 steps. Again, focus on keeping your legs straight and toes pointing forward. 
Really a great content. Let me tell you first about hip flexor it is the engine through which our body moves. They control balance, our ability to sit, stand, twist, reach, bend, walk and step. One of my patient also suffering from same problem but due to lack of money he was unable to afford a treatment. So i recommend him a program to unlock hip flexor. If anyone wants they can check it out here ;- https://tinyurl.com/y8yaqs2s Report
Premkumar et al present evidence that the traditional “red flags” for ominous causes of back pain can be quite misleading. The correlation between red flags and ominous diagnoses is poor, and prone to producing false negatives: that is, no red flags even when there is something more serious than unexplained pain going on. In a survey of almost 10,000 patients “the absence of red flag responses did not meaningfully decrease the likelihood of a red flag diagnosis.“ This is not even remotely a surprise to anyone who paid attention in back pain school, but it’s good to have some harder data on it.
En español | You probably know someone who’s traded a worn-out hip bone for ceramic or cobalt chrome. Some 370,000 Americans undergo hip-replacement surgery each year (the average age for this is 65). But the operation isn’t a cure-all: At least 1 in 10 hip-replacement recipients will need a second procedure to repair a dislocation, mechanical failure or infection. And hip pain, with or without surgery, can be a struggle. Chronic hip pain was a factor in the accidental opioid overdoses that claimed the lives of musicians Tom Petty, 66, and Prince, 57.
Sciatica is a form of radiculopathy caused by compression of the sciatic nerve, the large nerve that travels through the buttocks and extends down the back of the leg. This compression causes shock-like or burning low back pain combined with pain through the buttocks and down one leg, occasionally reaching the foot. In the most extreme cases, when the nerve is pinched between the disc and the adjacent bone, the symptoms may involve not only pain, but numbness and muscle weakness in the leg because of interrupted nerve signaling. The condition may also be caused by a tumor or cyst that presses on the sciatic nerve or its roots.
The hip flexors play an important role in everyday mobility and exercise. Involved in pulling the knee toward the hip, most movements either directly or indirectly use the hip flexors. That’s why even the slightest injury can cause great discomfort. Learn how you can recover from a hip flexor injury, and what precautions can be taken to avoid them.
Spinal laminectomy (also known as spinal decompression) is performed when spinal stenosis causes a narrowing of the spinal canal that causes pain, numbness, or weakness. During the procedure, the lamina or bony walls of the vertebrae, along with any bone spurs, are removed. The aim of the procedure is to open up the spinal column to remove pressure on the nerves. 
Along with these exercises, it's also important to do some supplementary exercises to work your hip's supporting muscles. You've probably heard of your shoulder's rotator cuff. Well, your hip also has a cuff, or a group of muscles that help stabilize and support movement. For these exercises, you'll need a mini-band, a longer thera-band or tubing (both are sold at many sporting goods stores, or can be purchased online), and a cable-column unit.
Two types of strength-training moves that may benefit the lower back are flexion and extension exercises. In flexion exercises, you bend forward to stretch the muscles of the back and hips. In extension exercises, you bend backward to develop the muscles that support the spine. One example is doing leg lifts while lying on your stomach. Depending on the cause of your back pain, there are some exercises you should not do. If you have back pain, make sure to talk to your doctor about what exercises are safe for you.
The JB Intensive Trainer Med Pro: A device that allows you to rehabilitate injury and pain, the JBIT MedPro helps strengthen hip muscles to alleviate pain over time. For older adults or those predisposed to joint and muscle conditions, the JBIT MedPro is an important preventative wellness solution, It can help mitigate the risk of worsened hip conditions that come with aging and wear and tear.
The good news is that there are plenty of good hip stretches out there that you can do to relieve discomfort, decrease tightness, and increase mobility in your hips. Since your hips are involved in so many of the movements you make (both inside and outside of the gym) stretching them is a great way to keep them feeling good and ready to work for you. Add some of the 12 hip stretches Atkins demos below to the end of your workout, or spend 10 minutes each day just doing a few of them, to improve mobility in your hips.
The big idea of classification-based cognitive functional therapy (CB-CFT or just CFT) is that most back pain has nothing to do with scary spinal problems and so the cycle of pain and disability can be broken by easing patient fears and anxieties. For this study, CFT was tried with 62 patients and compared to 59 who were treated with manual therapy and exercise. The CFT group did better: a 13-point boost on a 100-point disability scale, and 3 points on a 10-point pain scale. As the authors put it for BodyInMind.org, “Disabling back pain can change for the better with a different narrative and coping strategies.” These results aren’t proof that the confidence cure works, but they are promising.


