The diagnosis of low back pain involves a review of the history of the illness and underlying medical conditions as well as a physical examination. It is essential that a complete story of the back pain be reviewed including injury history, aggravating and alleviating conditions, associated symptoms (fever, numbness, tingling, incontinence, etc.), as well as the duration and progression of symptoms. Aside from routine abdomen and extremity evaluations, rectal and pelvic examinations may eventually be required as well. Further tests for diagnosis of low back pain can be required including blood and urine tests, plain film X-ray tests, CAT scanning, MRI scanning, bone scanning, and tests of the nerves such as electromyograms (EMG) and nerve conduction velocities (NCV).
Mechanical pain is often called back strain because it is linked with the movement, or "the mechanics" of the spine. This type of pain occurs when injury to the spine's discs, facet joints, ligaments, or muscles results in inflammation. It is called mechanical pain because it relates to the mechanics of your spine. The more you use your back, the more it hurts.
Veritas Health publishes original and accessible health related content written by more than 100 physician authors and peer-reviewed by a 16 member Medical Advisory Board. The Veritas Health platform comprising of Spine-health.com, Arthritis-health.com, Sports-health.com, and Pain-health.com, provides comprehensive information on back pain, arthritis, sports injuries, and chronic pain conditions. For more information visit Veritashealth.com.

While leg lifts, certain ab exercises, and even hula hooping can all help work the hips, the hip flexors can still be a tricky part of the body to stretch Kinetics of hula hooping: An inverse dynamics analysis. Cluff, T., Robertson, D.G., and Balasubramaniam, R. School of Human Kinetics, University of Ottawa, Ottawa, Ontario, Canada. Human Movement Science, 2008 Aug; 27 (4): 622-35.. To get them even stronger and more flexible, try these five simple hip flexor stretches:
A complete medical history and physical exam can usually identify any serious conditions that may be causing the pain. During the exam, a health care provider will ask about the onset, site, and severity of the pain; duration of symptoms and any limitations in movement; and history of previous episodes or any health conditions that might be related to the pain. Along with a thorough back examination, neurologic tests are conducted to determine the cause of pain and appropriate treatment. The cause of chronic lower back pain is often difficult to determine even after a thorough examination.
Acupuncture is no better than placebo, usual care, or sham acupuncture for nonspecific acute pain or sub-chronic pain.[87] For those with chronic pain, it improves pain a little more than no treatment and about the same as medications, but it does not help with disability.[87] This pain benefit is only present right after treatment and not at follow-up.[87] Acupuncture may be a reasonable method to try for those with chronic pain that does not respond to other treatments like conservative care and medications.[1][88]

How to: Get on your hands and knees, in a tabletop position (a). Slowly widen your knees out as far as they can go and bring your feet in line with your knees. Your shins should be parallel with one another (b). Flex your feet and ease yourself forward onto your forearms. (If the stretch is too intense, try putting your arms on a block or firm pillow.) Hold for eight to 12 breaths (c). If holding the stretch for longer, try slowly moving your hips forward and backward to bring the stretch to different parts of your hips.
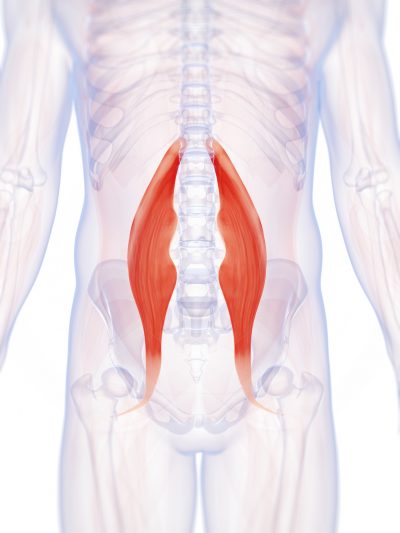
The multifidus muscles run up and down along the back of the spine, and are important for keeping the spine straight and stable during many common movements such as sitting, walking and lifting.[12] A problem with these muscles is often found in someone with chronic low back pain, because the back pain causes the person to use the back muscles improperly in trying to avoid the pain.[31] The problem with the multifidus muscles continues even after the pain goes away, and is probably an important reason why the pain comes back.[31] Teaching people with chronic low back pain how to use these muscles is recommended as part of a recovery program.[31]
At the very least, the tension and/or spasm in muscles that cross over the hip and attach onto the pelvis can contribute to imbalance, in terms of how strong and flexible each muscle group is in relation to the others. But muscle imbalance in the hips and the spine may make for pain, limitation and/or posture problems. It can also increase the healing challenge put to you by an existing injury or condition, for example, scoliosis.

Radicular pain. This type of pain can occur if a spinal nerve root becomes impinged or inflamed. Radicular pain may follow a nerve root pattern or dermatome down into the buttock and/or leg. Its specific sensation is sharp, electric, burning-type pain and can be associated with numbness or weakness (sciatica). It is typically felt on only one side of the body. 
Medications: A wide range of medications are used to treat acute and chronic low back pain. Some are available over the counter (OTC); others require a physician’s prescription. Certain drugs, even those available OTC, may be unsafe during pregnancy, may interact with other medications, cause side effects, or lead to serious adverse effects such as liver damage or gastrointestinal ulcers and bleeding. Consultation with a health care provider is advised before use. The following are the main types of medications used for low back pain:
Foraminotomy is an operation that “cleans out” or enlarges the bony hole (foramen) where a nerve root exits the spinal canal. Bulging discs or joints thickened with age can cause narrowing of the space through which the spinal nerve exits and can press on the nerve, resulting in pain, numbness, and weakness in an arm or leg. Small pieces of bone over the nerve are removed through a small slit, allowing the surgeon to cut away the blockage and relieve pressure on the nerve.
Low back pain has been with humans since at least the Bronze Age. The oldest known surgical treatise – the Edwin Smith Papyrus, dating to about 1500 BCE – describes a diagnostic test and treatment for a vertebral sprain. Hippocrates (c. 460 BCE – c. 370 BCE) was the first to use a term for sciatic pain and low back pain; Galen (active mid to late second century CE) described the concept in some detail. Physicians through the end of the first millennium did not attempt back surgery and recommended watchful waiting. Through the Medieval period, folk medicine practitioners provided treatments for back pain based on the belief that it was caused by spirits.[99]
Disc degeneration remains a key cause of chronic low back pain and the pain often persists despite surgery. NIH-funded basic science and preclinical studies are investigating molecular-level mechanisms that cause discs in the spine to degenerate, as well as protective mechanisms involved in disc remodeling that may diminish with advancing age. Such studies may help identify future therapeutic strategies to block degenerative mechanisms or promote remodeling processes. NIH also is funding early research on stem cell approaches to promote disc regeneration and rejuvenate cells of the nucleus pulposus, the jelly-like substance in the center of intervertebral discs that loses water content as people age.
Moist heat may help relax your muscles. Put moist heat on the sore area for 10 to 15 minutes at a time before you do warm-up and stretching exercises. Moist heat includes heat patches or moist heating pads that you can buy at most drugstores, a wet washcloth or towel that has been heated in a microwave or the dryer, or a hot shower. Don’t use heat if you have swelling.
Pregnancy commonly leads to low back pain by mechanically stressing the lumbar spine (changing the normal lumbar curvature) and by the positioning of the baby inside of the abdomen. Additionally, the effects of the female hormone estrogen and the ligament-loosening hormone relaxin may contribute to loosening of the ligaments and structures of the back. Pelvic-tilt exercises and stretches are often recommended for relieving this pain. Women are also recommended to maintain physical conditioning during pregnancy according to their doctors' advice. Natural labor can also cause low back pain.

But moving is important for hip and knee OA. It causes your joints to compress and release, bringing blood flow, nutrients, and oxygen into the cartilage. “This can help prolong the function and longevity of your joints,” says Eric Robertson, DPT, a physical therapist and associate professor of clinical physical therapy at the University of Southern California.
Health Tools Baby Due Date CalculatorBasal Metabolic Rate CalculatorBody Mass Index (BMI) CalculatorCalories Burned CalculatorChild Energy Requirements CalculatorDaily Calcium Requirements CalculatorDaily Fibre Requirements CalculatorIdeal Weight CalculatorInfectious Diseases Exclusion Periods ToolOvulation CalculatorSmoking Cost CalculatorTarget Heart Rate CalculatorWaist-to-hip Ratio Calculator Risk Tests Depression Self-AssessmentErectile Dysfunction ToolMacular Degeneration ToolOsteoporosis Risk TestProstate Symptoms Self-Assessment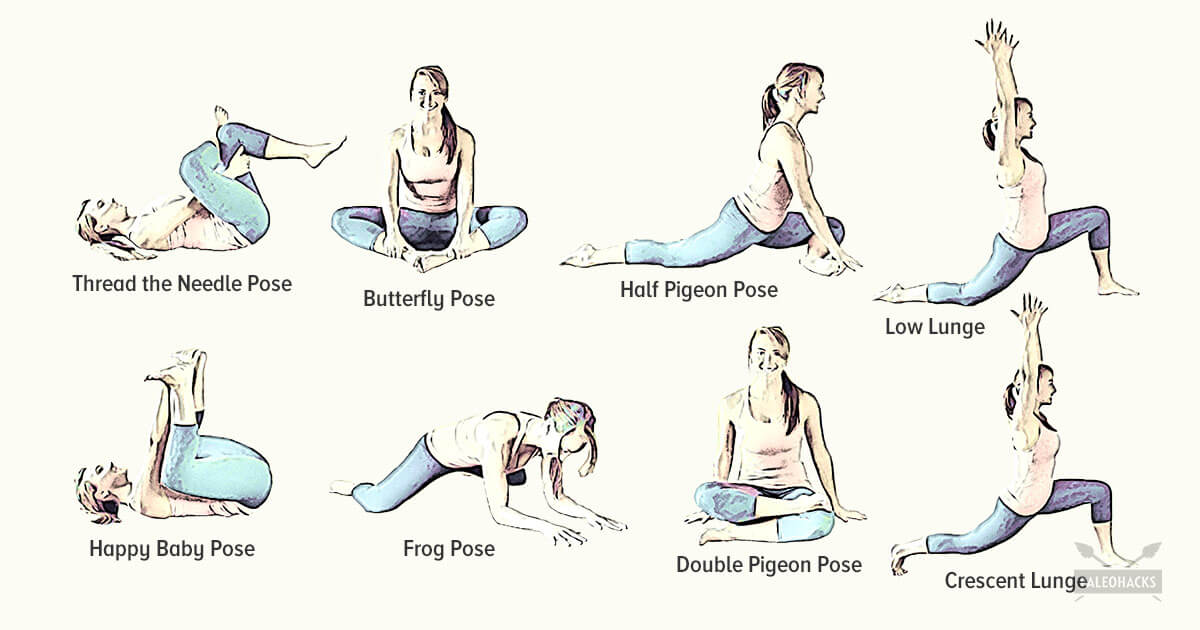
Endometriosis implants are most commonly found on the ovaries, the Fallopian tubes, outer surfaces of the uterus or intestines, and on the surface lining of the pelvic cavity. They also can be found in the vagina, cervix, and bladder. Endometriosis may not produce any symptoms, but when it does the most common symptom is pelvic pain that worsens just prior to menstruation and improves at the end of the menstrual period. Other symptoms of endometriosis include pain during sex, pain with pelvic examinations, cramping or pain during bowel movements or urination, and infertility.
Spinal manipulation and spinal mobilization are approaches in which professionally licensed specialists (doctors of chiropractic care) use their hands to mobilize, adjust, massage, or stimulate the spine and the surrounding tissues. Manipulation involves a rapid movement over which the individual has no control; mobilization involves slower adjustment movements. The techniques have been shown to provide small to moderate short-term benefits in people with chronic low back pain. Evidence supporting their use for acute or subacute low back pain is generally of low quality. Neither technique is appropriate when a person has an underlying medical cause for the back pain such as osteoporosis, spinal cord compression, or arthritis.
Back pain can suck the joy out of your days for week, months, even years. It can definitely be “serious” even when it’s not dangerous. I have worked with many truly miserable chronic low back pain patients, and of course the huge economic costs of back pain are cited practically anywhere the subject comes up. But your typical case of chronic low back pain, as nasty as it can be, has never killed anyone.

Really a great content. Let me tell you first about hip flexor it is the engine through which our body moves. They control balance, our ability to sit, stand, twist, reach, bend, walk and step. One of my patient also suffering from same problem but due to lack of money he was unable to afford a treatment. So i recommend him a program to unlock hip flexor. If anyone wants they can check it out here ;- https://tinyurl.com/y8yaqs2s Report
While leg lifts, certain ab exercises, and even hula hooping can all help work the hips, the hip flexors can still be a tricky part of the body to stretch Kinetics of hula hooping: An inverse dynamics analysis. Cluff, T., Robertson, D.G., and Balasubramaniam, R. School of Human Kinetics, University of Ottawa, Ottawa, Ontario, Canada. Human Movement Science, 2008 Aug; 27 (4): 622-35.. To get them even stronger and more flexible, try these five simple hip flexor stretches:
Veritas Health publishes original and accessible health related content written by more than 100 physician authors and peer-reviewed by a 16 member Medical Advisory Board. The Veritas Health platform comprising of Spine-health.com, Arthritis-health.com, Sports-health.com, and Pain-health.com, provides comprehensive information on back pain, arthritis, sports injuries, and chronic pain conditions. For more information visit Veritashealth.com.
I’m not endorsing or saying these stretches are a miracle cure, but I definitely think they’ve helped. I’ve even started to add a few gentle yoga poses and pilates moves which I could so easily do, back in the day, when I was 63 kilos and participated in the greatest oxymoron ever named … a thing called the Fun Run. If I’m not careful, and I keep stretching away each day, I could end up with a 6 pack and back to my 5′ 7″ instead of 5′ 5″.
I am a science writer and a former Registered Massage Therapist with a decade of experience treating tough pain cases. I was the Assistant Editor of ScienceBasedMedicine.org for several years. I’ve written hundreds of articles and several books, and I’m known for readable but heavily referenced analysis, with a touch of sass. I am a runner and ultimate player. • more about me • more about PainScience.com
Moist heat may help relax your muscles. Put moist heat on the sore area for 10 to 15 minutes at a time before you do warm-up and stretching exercises. Moist heat includes heat patches or moist heating pads that you can buy at most drugstores, a wet washcloth or towel that has been heated in a microwave or the dryer, or a hot shower. Don’t use heat if you have swelling.
2016 — More editing, more! Added some better information about pain being a poor indicator, and the role of myofascial trigger points. This article has become extremely busy in the last couple months — about 4,000 readers per day, as described here — so I am really polishing it and making sure that it’s the best possible answer to people’s fears about back pain.
Stop listening to other people’s horror stories. You know the scenario: You are bent over in obvious pain, waiting to see the doctor, and the person next to you tells you a 10-minute tale of how their Uncle Gordon had low back pain that required injections and surgery. But the pain still didn’t go away. Stop listening to these terrible stories. Most low back pain is short-lived and can be managed quite effectively with exercise and postural correction. Of course, some low back conditions are serious and require surgery, but that is a conversation you should have with your doctor, not the guy in the waiting room.
Lumbar herniated disc. The jelly-like center of a lumbar disc can break through the tough outer layer and irritate a nearby nerve root. The herniated portion of the disc is full of proteins that cause inflammation when they reach a nerve root, and inflammation as well as nerve compression cause nerve root pain. The disc wall is also richly supplied by nerve fibers, and a tear through the wall can cause severe pain.
Premkumar et al present evidence that the traditional “red flags” for ominous causes of back pain can be quite misleading. The correlation between red flags and ominous diagnoses is poor, and prone to producing false negatives: that is, no red flags even when there is something more serious than unexplained pain going on. In a survey of almost 10,000 patients “the absence of red flag responses did not meaningfully decrease the likelihood of a red flag diagnosis.“ This is not even remotely a surprise to anyone who paid attention in back pain school, but it’s good to have some harder data on it.
2016 — More editing, more! Added some better information about pain being a poor indicator, and the role of myofascial trigger points. This article has become extremely busy in the last couple months — about 4,000 readers per day, as described here — so I am really polishing it and making sure that it’s the best possible answer to people’s fears about back pain.

Bleeding in the pelvis is rare without significant trauma and is usually seen in patients who are taking blood-thinning medications, such as warfarin (Coumadin). In these patients, a rapid-onset sciatica pain can be a sign of bleeding in the back of the pelvis and abdomen that is compressing the spinal nerves as they exit to the lower extremities. Infection of the pelvis is infrequent but can be a complication of conditions such as diverticulosis, Crohn's disease, ulcerative colitis, pelvic inflammatory disease with infection of the Fallopian tubes or uterus, and even appendicitis. Pelvic infection is a serious complication of these conditions and is often associated with fever, lowering of blood pressure, and a life-threatening state.

Poor Sitting Posture: The correct position of your low back should have a slight forward curve called a lordosis. When you sit slouched, this lordosis straightens out-or even worse-reverses itself. This loss of the forward curve in your spine can cause increased pressure on the small shock absorbing discs in your back. This increased pressure can displace your discs and lead to low back pain. Your physical therapist can teach you the proper way to sit to decrease, eliminate, or prevent your back pain.
Long periods of inactivity in bed are no longer recommended, as this treatment may actually slow recovery. Spinal manipulation for periods of up to one month has been found to be helpful in some patients who do not have signs of nerve irritation. Future injury is avoided by using back-protection techniques during activities and support devices as needed at home or work.

When we stand, the lower back is functioning to support the weight of the upper body. When we bend, extend, or rotate at the waist, the lower back is involved in the movement. Therefore, injury to the structures important for weight bearing, such as the bony spine, muscles, tendons, and ligaments, often can be detected when the body is standing erect or used in various movements.
The diagnosis of low back pain involves a review of the history of the illness and underlying medical conditions as well as a physical examination. It is essential that a complete story of the back pain be reviewed including injury history, aggravating and alleviating conditions, associated symptoms (fever, numbness, tingling, incontinence, etc.), as well as the duration and progression of symptoms. Aside from routine abdomen and extremity evaluations, rectal and pelvic examinations may eventually be required as well. Further tests for diagnosis of low back pain can be required including blood and urine tests, plain film X-ray tests, CAT scanning, MRI scanning, bone scanning, and tests of the nerves such as electromyograms (EMG) and nerve conduction velocities (NCV).
2016 — More editing, more! Added some better information about pain being a poor indicator, and the role of myofascial trigger points. This article has become extremely busy in the last couple months — about 4,000 readers per day, as described here — so I am really polishing it and making sure that it’s the best possible answer to people’s fears about back pain.

Paget's disease of the bone is a condition of unknown cause in which the bone formation is out of synchrony with normal bone remodeling. This condition results in abnormally weakened bone and deformity and can cause localized bone pain, though it often causes no symptoms. Paget's disease is more common in people over the age of 50. Heredity (genetic background) and certain unusual virus infections have been suggested as causes. Thickening of involved bony areas of the lumbar spine can cause the radiating lower extremity pain of sciatica.
Meanwhile, it’s extremely common for non-life-threatening low back pain to be alarmingly severe and persistent — to have a loud bark! Your doctor may not appreciate how true this is, and may over-react to all persistent low back pain, even without other red flags. In most cases, you shouldn’t let them scare you. Being “freaked out” about persistent back pain is the real threat: it can make low back pain much worse, and much more likely to last even longer (a tragic irony).
Exercise therapy is effective in decreasing pain and improving function for those with chronic low back pain.[50] It also appears to reduce recurrence rates for as long as six months after the completion of program[61] and improves long-term function.[57] There is no evidence that one particular type of exercise therapy is more effective than another.[62] The Alexander technique appears useful for chronic back pain,[63] and there is tentative evidence to support the use of yoga.[64] Transcutaneous electrical nerve stimulation (TENS) has not been found to be effective in chronic low back pain.[65] Evidence for the use of shoe insoles as a treatment is inconclusive.[51] Peripheral nerve stimulation, a minimally-invasive procedure, may be useful in cases of chronic low back pain that do not respond to other measures, although the evidence supporting it is not conclusive, and it is not effective for pain that radiates into the leg.[66]
In the elderly, atherosclerosis can cause weakening of the wall of the large arterial blood vessel (aorta) in the abdomen. This weakening can lead to a bulging (aneurysm) of the aorta wall. While most aneurysms cause no symptoms, some cause a pulsating low back pain. Aneurysms of certain size, especially when enlarging over time, can require surgical repair with a grafting procedure to repair the abnormal portion of the artery.
Doing the bridge exercise in the morning gets your muscles working, activated, and engaged and will help support you the rest of the day, says Humphrey. Lie on your back with your legs bent and your feet flat on the floor, hip-width apart. Press down through your ankles and raise your buttocks off the floor while you tighten your abdominal muscles. Keep your knees aligned with your ankles and aim for a straight line from knees to shoulders, being sure not to arch your back; hold this position for three to five seconds and then slowly lower your buttocks back to the floor. Start with one set of 10 and build up to two or three sets.

One of the biggest dangers to your health is constantly sitting for long periods of time which can cause physical and emotional damage. 10 key moves that will help loosen your hip flexor and unlock the power within your body. There is an easy to follow program to unlocking your hip flexors that will strengthen your body, improve your health, and have an all day energy..... https://bit.ly/2HYTPrJ Report
Since the hip flexors are so easy to overuse and strain, it is important to stretch them before exercise or strenuous activity. Because of their connectedness to other muscle groups in the legs (like the quadriceps), it is important to stretch the muscle group as a whole, not individually. This ensures that the entire area is warmed up and ready for the strain of exercise or activity, not just one or two individual muscles.
If your hips are killing you, you probably spend a lot of time sitting – in the car, at work, on that spinning seat – which puts your hips in near-constant “flexion”, says Cori Lefkowith, NASM-certified personal trainer and owner of Redefining Strength in Orange County, California. Even running involves a repetitive flexion movement that can cause pain.


