The hip joint is designed to withstand a fair amount of wear and tear, but it’s not indestructible. For example, when you walk, a cushion of cartilage helps prevent friction as the hip bone moves in its socket. With age and use, this cartilage can wear down or become damaged, or the hip bone itself can be fractured during a fall. In fact, more than 300,000 adults over 65 are hospitalized for hip fractures each year, according to the Agency for Healthcare Research and Quality.

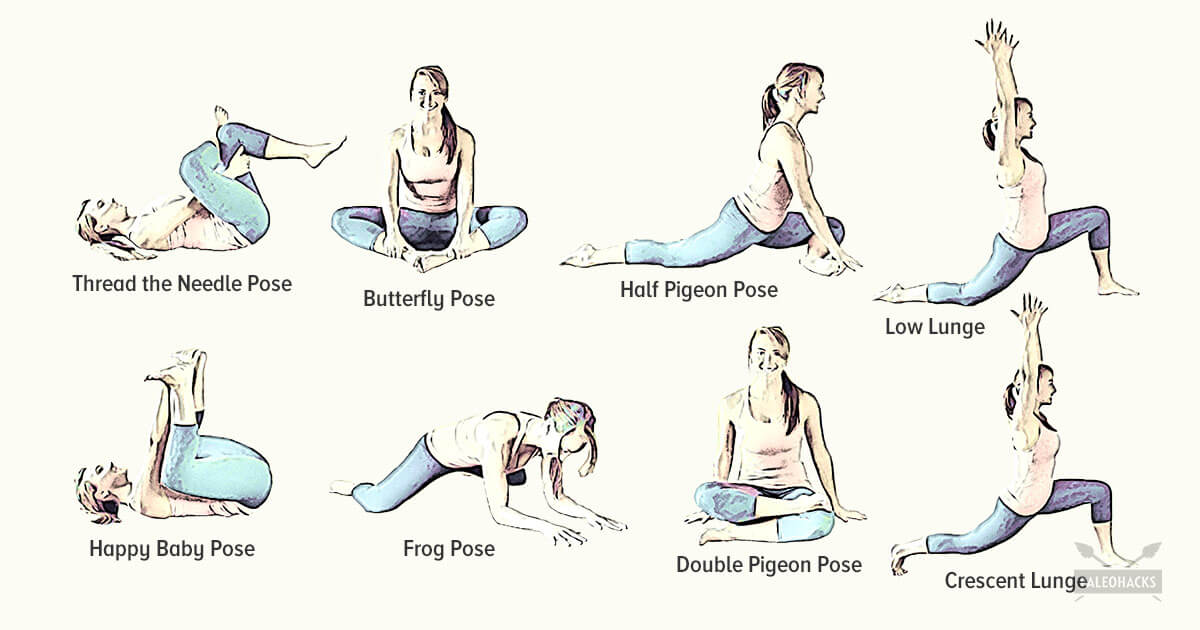
Following any period of prolonged inactivity, a regimen of low-impact exercises is advised. Speed walking, swimming, or stationary bike riding 30 minutes daily can increase muscle strength and flexibility. Yoga also can help stretch and strengthen muscles and improve posture. Consult a physician for a list of low-impact, age-appropriate exercises that are specifically targeted to strengthening lower back and abdominal muscles. 
Subacute low back pain. Lasting between 6 weeks and 3 months, this type of pain is usually mechanical in nature (such as a muscle strain or joint pain) but is prolonged. At this point, a medical workup may be considered, and is advisable if the pain is severe and limits one’s ability to participate in activities of daily living, sleeping, and working.
Fitness level: Back pain is more common among people who are not physically fit. Weak back and abdominal muscles may not properly support the spine. “Weekend warriors”—people who go out and exercise a lot after being inactive all week—are more likely to suffer painful back injuries than people who make moderate physical activity a daily habit. Studies show that low-impact aerobic exercise is beneficial for the maintaining the integrity of intervertebral discs.
Grade III (severe): A complete tear in your muscle that causes severe pain and swelling and you can't bear weight on that leg, making it difficult to walk. You've also lost more than 50 percent of your muscle function. These injuries are less common and may need surgery to repair the torn muscle. They can take several months or more to completely heal.
Exercise therapy is effective in decreasing pain and improving function for those with chronic low back pain.[50] It also appears to reduce recurrence rates for as long as six months after the completion of program[61] and improves long-term function.[57] There is no evidence that one particular type of exercise therapy is more effective than another.[62] The Alexander technique appears useful for chronic back pain,[63] and there is tentative evidence to support the use of yoga.[64] Transcutaneous electrical nerve stimulation (TENS) has not been found to be effective in chronic low back pain.[65] Evidence for the use of shoe insoles as a treatment is inconclusive.[51] Peripheral nerve stimulation, a minimally-invasive procedure, may be useful in cases of chronic low back pain that do not respond to other measures, although the evidence supporting it is not conclusive, and it is not effective for pain that radiates into the leg.[66]
Bridge: Still lying on your back with your feet flat on floor, lift your hips and torso off the floor into a bridge. Then interlace your hands underneath your hips and press your shoulders and upper arms into the floor, lifting your hips higher. Hold for 10 seconds. Lower yourself slowly back down, rolling down from the top of your spine to your tailbone. Repeat three times.

Sacroiliac joint dysfunction. The sacroiliac joint connects the sacrum at the bottom of the spine to each side of the pelvis. It is a strong, low-motion joint that primarily absorbs shock and tension between the upper body and the lower body. The sacroiliac joint can become painful if it becomes inflamed (sacroiliitis) or if there is too much or too little motion of the joint.
To help you strengthen these important muscles, Miranda put together a list of exercises, below. They include dynamic warm-up moves, meant to activate your hip muscles and prep them for the bigger movements to come; functional moves that train basic movement patterns, like the squat, hip hinge, and lunge; functional plyometric exercises that train explosive power; and a few moves that get you moving in different planes of motion, or directions.
Cycling: The repetitive movements of cycling can place a strain on your hip joints, not to mention that it can also affect your posture! If you really must cycle, make sure your bike is professionally fitted and that you properly warm up and stretch your hip flexors before getting on your bike. I’d recommend choosing an alternative though, or at least speaking to your doctor first!
Stop listening to other people’s horror stories. You know the scenario: You are bent over in obvious pain, waiting to see the doctor, and the person next to you tells you a 10-minute tale of how their Uncle Gordon had low back pain that required injections and surgery. But the pain still didn’t go away. Stop listening to these terrible stories. Most low back pain is short-lived and can be managed quite effectively with exercise and postural correction. Of course, some low back conditions are serious and require surgery, but that is a conversation you should have with your doctor, not the guy in the waiting room.

Health Tools Baby Due Date CalculatorBasal Metabolic Rate CalculatorBody Mass Index (BMI) CalculatorCalories Burned CalculatorChild Energy Requirements CalculatorDaily Calcium Requirements CalculatorDaily Fibre Requirements CalculatorIdeal Weight CalculatorInfectious Diseases Exclusion Periods ToolOvulation CalculatorSmoking Cost CalculatorTarget Heart Rate CalculatorWaist-to-hip Ratio Calculator Risk Tests Depression Self-AssessmentErectile Dysfunction ToolMacular Degeneration ToolOsteoporosis Risk TestProstate Symptoms Self-Assessment

The National Institute of Neurological Disorders and Stroke (NINDS) is a component of the National Institutes of Health (NIH) and is the leading federal funder of research on disorders of the brain and nervous system. As a primary supporter of research on pain and pain mechanisms, NINDS is a member of the NIH Pain Consortium, which was established to promote collaboration among the many NIH Institutes and Centers with research programs and activities addressing pain. On an even broader scale, NIH participates in the Interagency Pain Research Coordinating Committee, a federal advisory committee that coordinates research across other U.S. Department of Health and Human Services agencies as well as the Departments of Defense and Veterans Affairs.
Congenital bone conditions: Congenital causes (existing from birth) of low back pain include scoliosis and spina bifida. Scoliosis is a sideways (lateral) curvature of the spine that can be caused when one lower extremity is shorter than the other (functional scoliosis) or because of an abnormal architecture of the spine (structural scoliosis). Children who are significantly affected by structural scoliosis may require treatment with bracing and/or surgery to the spine. Adults infrequently are treated surgically but often benefit by support bracing. Spina bifida is a birth defect in the bony vertebral arch over the spinal canal, often with absence of the spinous process. This birth defect most commonly affects the lowest lumbar vertebra and the top of the sacrum. Occasionally, there are abnormal tufts of hair on the skin of the involved area. Spina bifida can be a minor bony abnormality without symptoms. However, the condition can also be accompanied by serious nervous abnormalities of the lower extremities.

Lie on your back with your knees bent and your feet flat on the floor. Tighten your buttocks and lift your hips off the floor. Tighten your abdominal muscles and lift one foot a couple of inches off the floor. Then put it down and lift the other foot a couple of inches, all while remembering to breathe. “It’s like taking alternate steps,” Pariser says. Work up to doing 30 steps at a time.
Spondylolisthesis. This condition occurs when one vertebra slips over the adjacent one. There are 5 types of spondylolisthesis but the most common are secondary to a defect or fracture of the pars (between the facet joints) or mechanical instability of the facet joints (degenerative). The pain can be caused by instability (back) or compression of the nerves (leg).
Beacon Orthopaedics & Sports Medicine, Ltd. complies with applicable Federal civil rights laws and does not discriminate on the basis of race, color, national origin, age, disability, or sex. If you speak a language other than English, language assistance services, free of charge, are available to you. Call the Call Center at (513) 354-3700. Español (Spanish): ATENCIÓN: Si habla español, tiene a su disposición servicios gratuitos de asistencia lingüística. Llame al Call Center at (513) 354-3700. 繁體中文 (Chinese): 注意:如果您使用繁體中文,您可以免費獲得語言援助服務。請致電 Call Center at (513) 354-3700.
In the vast majority of patients with low back pain, symptoms can be attributed to nonspecific mechanical factors. However, in a much smaller percentage of patients, the cause of back pain may be something more serious, such as cancer, cauda equina syndrome, spinal infection, spinal compression fractures, spinal stress fractures, ankylosing spondylitis, or aneurysm.
Mechanical pain. By far the most common cause of lower back pain, mechanical pain (axial pain) is pain primarily from the muscles, ligaments, joints (facet joints, sacroiliac joints), or bones in and around the spine. This type of pain tends to be localized to the lower back, buttocks, and sometimes the top of the legs. It is usually influenced by loading the spine and may feel different based on motion (forward/backward/twisting), activity, standing, sitting, or resting.
There is a significant overlap of nerve supply to many of the discs, muscles, ligaments, and other spinal structures, and it can be difficult for the brain to accurately sense which is the cause of the pain. For example, a degenerated or torn lumbar disc can feel the same as a pulled muscle – both creating inflammation and painful muscle spasm in the same area. Muscles and ligaments heal rapidly, while a torn disc may or may not. The time course of pain helps determine the cause. 
Magnetic resonance imaging (MRI) uses a magnetic force instead of radiation to create a computer-generated image. Unlike x-ray, which shows only bony structures, MRI scans also produce images of soft tissues such as muscles, ligaments, tendons, and blood vessels. An MRI may be ordered if a problem such as infection, tumor, inflammation, disc herniation or rupture, or pressure on a nerve is suspected. MRI is a noninvasive way to identify a condition requiring prompt surgical treatment. However, in most instances, unless there are “red flags” in the history or physical exam, an MRI scan is not necessary during the early phases of low back pain.
3. Tendinitis and bursitis Many tendons around the hip connect the muscles to the joint. These tendons can easily become inflamed if you overuse them or participate in strenuous activities. One of the most common causes of tendinitis at the hip joint, especially in runners, is iliotibial band syndrome — the iliotibial band is the thick span of tissue that runs from the outer rim of your pelvis to the outside of your knee.
The hip is a very stable ball and socket type joint with an inherently large range of motion. The hip contains some of the largest muscle in the body as well as some of the smallest. Most people lack mobility due to a relatively sedentary lifestyle. Periods of prolonged sitting results in tightness of the hip flexors and hamstrings. Tightness in the muscles and ligaments can created joint forces that result in arthritis, postural problems, bursitis, and mechanical back pain.
When was the last time you got on your gym's abductor or adductor machine and got in a good workout? It's probably been a while. Both are machines that don't get a lot of use, and they are often the target of coaches' ridicule on those "useless gym moves we should all skip" lists. Perhaps rightly so, especially if you're hopping on those machines hoping for a slimming effect.

People routinely have no pain despite the presence of obvious arthritic degeneration, herniated discs, and other seemingly serious structural problems like stenosis and spondylolistheses. This surprising contradiction has been made clear by a wide variety of research over the years, but the most notable in recent history is Brinjikji 2015. There are painful spinal problems, of course — which was also shown by Brinjikji et al in a companion paper — but they are mostly more rare and unpredictable than most people suspect, and there are many fascinating examples of people who “should” be in pain but are not, and vice versa. Spinal problems are only one of many ingredients in back pain. BACK TO TEXT
The hips are one of those body parts that most of us don't really think about until they're bothering us. When you hit the gym, strengthening your hip muscles specifically probably isn't high on the agenda. But if you're someone who spends most days sitting, you're likely familiar with that hip ache and tightness that comes along with it. Maybe you've even started doing some hip stretches to combat that. But actually strengthening the hip area is something that will not only make you feel better, but help you move better, too.
Putting the exercise in writing do not help me, I need to watch them doing them so, I can figer out how to do them, or if I should even try to do them. I use the flex extendors, lifting my legs one at a time from the flor to strengthen my thys, hip and buttox. And I try to remember to do the bridge excerise. I have had 2 total hip replacements , 7 months a part, in 2013. Trying to get stronger with cold weather will be 70 in Feb. Linda
When I do a deep knee bend like a sumo squat I get a popping in the outside of my left knee. It feels like a big tendon or ligament is slipping per something. It isn’t painful peer se but I’m afraid if I do it a lot it will be. Is that a relatively common symptom for a guy with tight flexors, it bands, etc? Should I just push through it or have it checked out?
How to: Lie on your back with your right knee bent and foot flat on the floor (a). Extend your left leg up to the ceiling and wrap a strap around the sole of your left foot (b). While holding both ends with your left hand, extend your right arm directly out to the side in order to anchor yourself (c). Slowly let the left leg fall toward the left while keeping your right side grounded. Hold for six to eight breaths, then repeat on the opposite side.


Moist heat may help relax your muscles. Put moist heat on the sore area for 10 to 15 minutes at a time before you do warm-up and stretching exercises. Moist heat includes heat patches or moist heating pads that you can buy at most drugstores, a wet washcloth or towel that has been heated in a microwave or the dryer, or a hot shower. Don’t use heat if you have swelling.

Or anything else. Pain is a poor indicator, period! The human nervous system is really terrible about this: it routinely produces false alarms, and alarms that are much too loud. See Pain is Weird: Pain science reveals a volatile, misleading sensation that is often more than just a symptom, and sometimes worse than whatever started it. BACK TO TEXT

As with any sort of pain, it's crucial to figure out the source so you can properly treat it. Sharp or stabbing pain that extends beyond your low back or is accompanied by symptoms like abdominal pain, nausea, and vomiting, could be signs of various other conditions and definitely warrant a trip to the doctor. If you have a history of lower back injuries or disc problems, always see your doctor before trying any new exercise.
The hip is a basic ball-and-socket joint. The ball is the femoral head—a knob on the top of the thigh bone—and the socket is an indentation in the pelvic bone. There is cartilage lining the joint (called the labrum) and ligaments that attach the pelvic and thigh bones. Numerous muscles attach around the hip, too, moving the joint through the basic motions of flexion (bending), extension (extending the leg behind you), abduction (lifting the leg away from the body), adduction (moving the leg inward), internal rotation, and external rotation.
Apply the above concept to your hips. When you sit, your hips are in a "flexed" position. Therefore, the muscles that flex your hips are in a shortened state. You probably spend at least a third of your day sitting down. Think about how much time those hip flexor muscles stay shortened. A lot. Over time, they become tighter and tighter until you look like the old man in the picture. So unless you want to look like that, perform the stretches shown below.
Activity: Bed rest should be limited. Individuals should begin stretching exercises and resume normal daily activities as soon as possible, while avoiding movements that aggravate pain. Strong evidence shows that persons who continue their activities without bed rest following onset of low back pain appeared to have better back flexibility than those who rested in bed for a week. Other studies suggest that bed rest alone may make back pain worse and can lead to secondary complications such as depression, decreased muscle tone, and blood clots in the legs.
Six sciatica stretches for pain relief Sciatica is nerve pain that runs through the buttocks, down the back of the leg and into the ankle or foot. It is a symptom of several different back, pelvis, and hip problems, and can also occur as a result of pregnancy. Stretching can provide relief from the pain. Here, we suggest six stretches to perform every day. Read now
Iliopsoas syndrome, which is also called psoas syndrome or iliopsoas tendonitis, occurs when the iliopsoas muscles are injured. Lower back pain is the most common symptom; however, pain can also occur in the hip, thigh, or leg. The iliopsoas bursa, which is a fluid-filled sac located on the inside of the hip that reduces rubbing and friction, is also likely to become inflamed due to the proximity of the two structures. When this happens, the inflamed bursae will make it difficult to move.
The condition is cauda equina syndrome. It involves “acute loss of function of the neurologic elements (nerve roots) of the spinal canal below the termination (conus) of the spinal cord,” where the nerves spread out like a horse (equina) tail. Again, this condition causes symptoms in the “saddle” of the body: butt, groin, inner thighs. BACK TO TEXT
When I do a deep knee bend like a sumo squat I get a popping in the outside of my left knee. It feels like a big tendon or ligament is slipping per something. It isn’t painful peer se but I’m afraid if I do it a lot it will be. Is that a relatively common symptom for a guy with tight flexors, it bands, etc? Should I just push through it or have it checked out?
Sit in a chair with good lumbar support and proper position and height for the task. Keep shoulders back. Switch sitting positions often and periodically walk around the office or gently stretch muscles to relieve tension. A pillow or rolled-up towel placed behind the small of the back can provide some lumbar support. During prolonged periods of sitting, elevate feet on a low stool or a stack of books.
Physician specialties that evaluate and treat low back pain range from generalists to subspecialists.These specialties include emergency medicine physicians, general medicine, family medicine, internal medicine, gynecology, spine surgeons (orthopaedics and neurosurgery), rheumatology, pain management, and physiatry. Other health care providers for low back pain include physical therapists, chiropractors, massage therapists, psychologists, and acupuncturists.
Magnetic resonance imaging (MRI) uses a magnetic force instead of radiation to create a computer-generated image. Unlike x-ray, which shows only bony structures, MRI scans also produce images of soft tissues such as muscles, ligaments, tendons, and blood vessels. An MRI may be ordered if a problem such as infection, tumor, inflammation, disc herniation or rupture, or pressure on a nerve is suspected. MRI is a noninvasive way to identify a condition requiring prompt surgical treatment. However, in most instances, unless there are “red flags” in the history or physical exam, an MRI scan is not necessary during the early phases of low back pain.
Fitness level: Back pain is more common among people who are not physically fit. Weak back and abdominal muscles may not properly support the spine. “Weekend warriors”—people who go out and exercise a lot after being inactive all week—are more likely to suffer painful back injuries than people who make moderate physical activity a daily habit. Studies show that low-impact aerobic exercise is beneficial for the maintaining the integrity of intervertebral discs.
Neglect your lower body too often and you risk losing mobility — that thing that allows you to plop down on the floor to play with your kids, or get up and out of even the cushiest chair with ease. “A lot of people sit all day, so they’re not necessarily using their glute muscles,” says Daily Burn Fitness/Nutrition Coach Allie Whitesides. “And a lot of people are in the car all the time, so we’re not using our leg muscles much, either.”

Blood tests are not routinely used to diagnose the cause of back pain; however in some cases they may be ordered to look for indications of inflammation, infection, and/or the presence of arthritis. Potential tests include complete blood count, erythrocyte sedimentation rate, and C-reactive protein. Blood tests may also detect HLA-B27, a genetic marker in the blood that is more common in people with ankylosing spondylitis or reactive arthritis (a form of arthritis that occurs following infection in another part of the body, usually the genitourinary tract).
There are cases of low back pain that have alarming causes, but it’s rare. Once in a while back pain is a warning sign of cancer, autoimmune disease, infection, or a handful of other scary culprits.7 Over the age of 55, about one in twenty cases turns out to be a fracture, and one in a hundred is more ominous.8 The further you are from 55, the better your odds.
In both younger and older patients, vertebral fractures take weeks to heal with rest and pain relievers. Compression fractures of vertebrae associated with osteoporosis can also be treated with a procedure called vertebroplasty or kyphoplasty, which can help to reduce pain. In this procedure, a balloon is inflated in the compressed vertebra, often returning some of its lost height. Subsequently, a "cement" (methymethacrylate) is injected into the balloon and remains to retain the structure and height of the body of the vertebra. Pain is relieved as the height of the collapsed vertebra is restored.
Multiple sclerosis (MS) symptoms vary from person to person, and can last for days to months without periods of remission. Symptoms of MS include sexual problems and problems with the bowel, bladder, eyes, muscles, speech, swallowing, brain, and nervous system. The early symptoms and signs of multiple sclerosis usually start between age 20 and 40. MS in children, teens, and those over age 40 is rare. Treatment options for multiple sclerosis vary depending on the type and severity of symptoms. Medications may be prescribed to manage MS symptoms.
Place a mini band around your ankles and spread your feet about shoulder-width apart. Keeping your legs relatively straight (you want the motion to come from your hips) and toes pointing forward, walk forward 10 steps, then backward 10 steps. Take a short break and then walk to the right 10 steps, then to the left 10 steps. Again, focus on keeping your legs straight and toes pointing forward.
Physician specialties that evaluate and treat low back pain range from generalists to subspecialists.These specialties include emergency medicine physicians, general medicine, family medicine, internal medicine, gynecology, spine surgeons (orthopaedics and neurosurgery), rheumatology, pain management, and physiatry. Other health care providers for low back pain include physical therapists, chiropractors, massage therapists, psychologists, and acupuncturists.

Located deep in the front of the hip and connecting the leg, pelvis, and abdomen, the hip flexors— surprise, surprise— flex the hip. But despite being some of the most powerful muscles in our bodies (with a clearly important role), it’s easy to neglect our poor hip flexors— often without even knowing it. It turns out just working at a desk all day (guilty!) can really weaken hip flexors since they tend to shorten up while in a seated position. This tightness disrupts good posture and is a common cause of lower back pain. Weakened hip flexors can also increase the risk of foot, ankle, and knee injuries (especially among runners) Hip muscle weakness and overuse injuries in recreational runners. Niemuth, P.E., Johnson, R.J., Myers, M.J., et al. Rocky Mountain University of Health Professions, Provo, VT. Clinical Journal of Sport Medicine, 2005 Jan; 15 (1): 14-21.. So be sure to get up, stand up every hour or so! And giving the hip flexors some extra attention is not just about injury prevention. Adding power to workouts, working toward greater flexibility, and getting speedier while running is also, as they say, all in the hips The effect of walking speed on muscle function and mechanical energetics. Neptune, R.R., Sasaki, K., and Kautz, S.A. Department of Mechanical Engineering, The University of Texas, Austin, TX. Gait & Posture, 2008 Jul; 28 (1): 135-43..


