Prolonged sitting and activities like running or cycling can lead to tight hip flexor muscles and a variety of skeletal imbalances. Think: if you only cycle for exercise, certain muscles in your legs will get stronger (in a lot of cases you overwork these muscles) yet your core and outer hip muscles might get weaker from lack of engagement. So what? Well, these muscle imbalances often lead to skeletal imbalances and injuries down the line. If you have particularly tight hip flexors, your body will start to create an anterior pull on the pelvis (anterior pelvic tilt). You can identify an anterior pelvic tilt if your belly protrudes slightly in the front while your butt sticks out in the back (what some people refer to as “duck butt”).
Im a skateboarder and a couple weeks ago i skated alot every day and my lefy hip was starting to get sore. But of course i couldnt resist skating so i kept skating and it got worse and worse to the point i couldnt really skate at all without my hip hurting but of course i would still mess around on the board doing tiny tricks but a couple days ago i was just skating around not really doing tricks and i slipped and kicked my leg out and REALLY hurt my hip and thought i tore a tendon or something and couldnt walk for two days, but its gotten alot better and i can walk fairly normal and i ice it everyday but whenever i stretch it its just a really sharp pain it doesnt feel like im stretching it. What do i do when all the stretch does is make a sharp pain? How do i strengthen my hip? And how long would it take to strengthen my hip to full strength again? Because i cant stand not being able to skate. Please reply so i can skate as soon as possible thank you
Before recommending exercises, physical therapists evaluate their patients to develop a routine that’s appropriate for their specific condition. Pariser says the following exercises, done at home and at the gym, are generally safe for everyone. “If a patient has already received a total hip replacement, however, certain precautions should be taken,” he says.
Long periods of inactivity in bed are no longer recommended, as this treatment may actually slow recovery. Spinal manipulation for periods of up to one month has been found to be helpful in some patients who do not have signs of nerve irritation. Future injury is avoided by using back-protection techniques during activities and support devices as needed at home or work.

The Child’s Pose is a yoga position that is especially beneficial for the back. To perform Child’s Pose, start on all fours, then stretch back, resting your bottom on your feet. Your arms should stay extended with your hands on the floor. This creates a stretch in your lower back. Hold this pose for 30 seconds, then return to your starting position. Repeat five times.
When you tell your doctor your hip hurts, the first thing she should do is confirm that your hip is actually the problem. Women might say they have hip pain, but what they may mean is that they have pain in the side of the upper thigh or upper buttock, or they may be experiencing lower back pain, says Stephanie E. Siegrist, MD, an orthopedic surgeon in Rochester, New York, and a spokeswoman for the American Academy of Orthopaedic Surgeons. Hip pain is often felt in the groin or on the outside of the hip directly over where the hip joint (a ball-and-socket joint) is located.
The side of the pain on its own doesn’t tell us much, and most of the one-sided sources of pain are viscera that usually cause abdominal pain instead of back pain, or in addition to it. In other words, the only reason to worry about right or left lower back pain is if it is otherwise worrisome: if you have other red flags or significant non-back symptoms.
Physician specialties that evaluate and treat low back pain range from generalists to subspecialists.These specialties include emergency medicine physicians, general medicine, family medicine, internal medicine, gynecology, spine surgeons (orthopaedics and neurosurgery), rheumatology, pain management, and physiatry. Other health care providers for low back pain include physical therapists, chiropractors, massage therapists, psychologists, and acupuncturists.
Fitness level: Back pain is more common among people who are not physically fit. Weak back and abdominal muscles may not properly support the spine. “Weekend warriors”—people who go out and exercise a lot after being inactive all week—are more likely to suffer painful back injuries than people who make moderate physical activity a daily habit. Studies show that low-impact aerobic exercise is beneficial for the maintaining the integrity of intervertebral discs.
For example, your quadriceps muscles are a group of four that are located at the front of the thigh; one of the group members, the rectus femoris flexes the hip, which brings your lower extremity (thigh, lower leg, and foot) forward, in front of you. On the other hand, your hamstring muscles are located at the back of the thigh. When they contract, they extend the lower extremity, bringing it behind you.

MRI (or magnetic resonance imaging) scan is a radiology technique which uses magnetism, radio waves, and a computer to produce images of body structures. MRI scanning is painless and does not involve X-ray radiation. Patients with heart pacemakers, metal implants, or metal chips or clips in or around the eyes cannot be scanned with MRI because of the effect of the magnet.
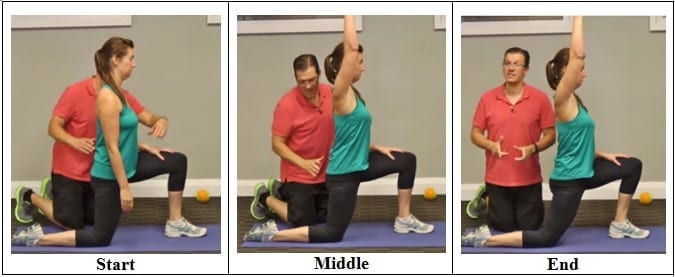
Since the hip flexors are so easy to overuse and strain, it is important to stretch them before exercise or strenuous activity. Because of their connectedness to other muscle groups in the legs (like the quadriceps), it is important to stretch the muscle group as a whole, not individually. This ensures that the entire area is warmed up and ready for the strain of exercise or activity, not just one or two individual muscles.
Degenerative bone and joint conditions: As we age, the water and protein content of the body's cartilage changes. This change results in weaker, thinner, and more fragile cartilage. Because both the discs and the joints that stack the vertebrae (facet joints) are partly composed of cartilage, these areas are subject to wear and tear over time (degenerative changes). Degeneration of the disc is called spondylosis. Spondylosis can be noted on X-rays of the spine as a narrowing of the normal "disc space" between the vertebrae. It is the deterioration of the disc tissue that predisposes the disc to herniation and localized lumbar pain ("lumbago") in older patients. Degenerative arthritis (osteoarthritis) of the facet joints is also a cause of localized lumbar pain that can be detected with plain X-ray testing. These causes of degenerative back pain are usually treated conservatively with intermittent heat, rest, rehabilitative exercises, and medications to relieve pain, muscle spasm, and inflammation.
Swimming is a low impact form of exercise that can help to relieve the pressure on your joints. It’s thought that water aerobics may help to reduce the impact on your joints by up to 75%!2 Be careful though; start with a beginner’s class and always do only what you’re comfortable with – try to avoid over-exercising or pushing your muscles too far!
To ease the pain and lower your odds of an injury, don’t try to do too much at once. “Start with just 10 minutes,” says Arina Garg, MD, a rheumatology fellow at The Center for Excellence for Arthritis and Rheumatology at the Louisiana University Health Sciences Center. “Every few days, increase that time by 5 to 10 minutes.” Your goal is to work up to 30 minutes of aerobic exercise, 5 days a week.
To understand various causes of low back pain, it is important to appreciate the normal design (anatomy) of the tissues of this area of the body. Important structures of the low back that can be related to symptoms in this region include the bony lumbar spine (vertebrae, singular = vertebra), discs between the vertebrae, ligaments around the spine and discs, spinal cord and nerves, muscles of the low back, internal organs of the pelvis and abdomen, and the skin covering the lumbar area.
Bony encroachment: Any condition that results in movement or growth of the vertebrae of the lumbar spine can limit the space (encroachment) for the adjacent spinal cord and nerves. Causes of bony encroachment of the spinal nerves include foraminal narrowing (narrowing of the portal through which the spinal nerve passes from the spinal column, out of the spinal canal to the body, commonly as a result of arthritis), spondylolisthesis (slippage of one vertebra relative to another), and spinal stenosis (compression of the nerve roots or spinal cord by bony spurs or other soft tissues in the spinal canal). Spinal-nerve compression in these conditions can lead to sciatica pain that radiates down the lower extremities. Spinal stenosis can cause lower-extremity pains that worsen with walking and are relieved by resting (mimicking the pains of poor circulation). Treatment of these afflictions varies, depending on their severity, and ranges from rest and exercises to epidural cortisone injections and surgical decompression by removing the bone that is compressing the nervous tissue.

Nerve irritation: The nerves of the lumbar spine can be irritated by mechanical pressure (impingement) by bone or other tissues, or from disease, anywhere along their paths -- from their roots at the spinal cord to the skin surface. These conditions include lumbar disc disease (radiculopathy), bony encroachment, and inflammation of the nerves caused by a viral infection (shingles). See descriptions of these conditions below.

You could do these moves all together as a single workout, or, as Miranda suggests, split them in half and do the first part one day and the second part another—"but do the warm-up with each one," she says. Those first three moves are meant to not only "wake up" the muscles, but also get your brain ready for the movement patterns to come. For that reason, she says that doing the first three moves "would be a fantastic warm-up before any workout."

Stop listening to other people’s horror stories. You know the scenario: You are bent over in obvious pain, waiting to see the doctor, and the person next to you tells you a 10-minute tale of how their Uncle Gordon had low back pain that required injections and surgery. But the pain still didn’t go away. Stop listening to these terrible stories. Most low back pain is short-lived and can be managed quite effectively with exercise and postural correction. Of course, some low back conditions are serious and require surgery, but that is a conversation you should have with your doctor, not the guy in the waiting room.
Chronic back pain is defined as pain that persists for 12 weeks or longer, even after an initial injury or underlying cause of acute low back pain has been treated. About 20 percent of people affected by acute low back pain develop chronic low back pain with persistent symptoms at one year. In some cases, treatment successfully relieves chronic low back pain, but in other cases pain persists despite medical and surgical treatment.
The only activity performed on a regular basis that fully extends the hip is walking and running. Hence as activity levels decrease so does the ability to extend the hip. This results in compensatory pelvic tilting and lumbar extension, with a reduction in the ability to accommodate uneven ground, negotiate obstacles, or attempt to change walking speed quickly. The compensatory pelvic tilt that accompanies tight hip flexors also predisposes the individual to postural problems and back pain. Hip stretches done on a regular basis can help you maintain extension range of motion and thereby improve function.
^ Enke, Oliver; New, Heather A.; New, Charles H.; Mathieson, Stephanie; McLachlan, Andrew J.; Latimer, Jane; Maher, Christopher G.; Lin, C.-W. Christine (2 July 2018). "Anticonvulsants in the treatment of low back pain and lumbar radicular pain: a systematic review and meta-analysis". Canadian Medical Association Journal. 190 (26): E786–E793. doi:10.1503/cmaj.171333. PMC 6028270. PMID 29970367. 
myDr myDr provides comprehensive Australian health and medical information, images and tools covering symptoms, diseases, tests, medicines and treatments, and nutrition and fitness.Related ArticlesSciatica: symptoms, causes and diagnosisSciatica is characterised by pain deep in the buttock often radiating down the back of the leg. One Sciatica: treatmentMost sciatica gets better within a few weeks. If not, there are treatments that may help relieve youNeck pain: symptoms and causesKnowing the symptoms of your neck pain and when to see a doctor can help in finding the cause and geNeck pain: treatmentTreatment for neck pain depends on the cause and how severe it is. Neck pain treatment, includiOffice ergonomics: workstation comfort and safetyComputer users often develop aches and pains. Avoid discomfort by setting up your workstation accordPilates no better for low back painCochrane researchers found no significant difference between Pilates and other exercises for pain anDormant butt syndrome is linked to knee and back painDormant butt syndrome, characterised by weak glute muscles and tight hip flexors, can be caused by sSpinal surgery for low back pain over-optimisticSpinal fusion surgery has at best a 50% success rate for the initial operation and patients would beVideo: Reframing pain to overcome lower back painReliance on opioid painkillers and unnecessary back surgeries may be preventing us from beating loweAdvertisement
Lumbar radiculopathy: Lumbar radiculopathy is nerve irritation that is caused by damage to the discs between the vertebrae. Damage to the disc occurs because of degeneration ("wear and tear") of the outer ring of the disc, traumatic injury, or both. As a result, the central softer portion of the disc can rupture (herniate) through the outer ring of the disc and abut the spinal cord or its nerves as they exit the bony spinal column. This rupture is what causes the commonly recognized "sciatica" pain of a herniated disc that shoots from the low back and buttock down the leg. Sciatica can be preceded by a history of localized low-back aching or it can follow a "popping" sensation and be accompanied by numbness and tingling. The pain commonly increases with movements at the waist and can increase with coughing or sneezing. In more severe instances, sciatica can be accompanied by incontinence of the bladder and/or bowels. The sciatica of lumbar radiculopathy typically affects only one side of the body, such as the left side or right side, and not both. Lumbar radiculopathy is suspected based on the above symptoms. Increased radiating pain when the lower extremity is lifted supports the diagnosis. Nerve testing (EMG/electromyogramspina bifida
Stop focusing on a specific diagnosis. Up to 85% of low back pain can be classified as "non-specific." This means that the origin of your pain cannot be localized to one specific structure or problem. While common diagnostic tests for low back pain can show the bones, discs, and joints with great detail, no test can tell the exact cause of your pain with 100% accuracy.

Some of these red flags are much less red than others, especially depending on the circumstances. For instance, “weight loss” is common and often the sign of successful diet! (Well, at least temporarily successful, anyway. 😃) Obviously, if you know of a harmless reason why you have a red flag symptom, it isn’t really a red flag (duh!). But every single actual red flag — in combination with severe low back pain that’s been going on for several weeks — is definitely a good reason to get yourself checked out.
Prolonged sitting and activities like running or cycling can lead to tight hip flexor muscles and a variety of skeletal imbalances. Think: if you only cycle for exercise, certain muscles in your legs will get stronger (in a lot of cases you overwork these muscles) yet your core and outer hip muscles might get weaker from lack of engagement. So what? Well, these muscle imbalances often lead to skeletal imbalances and injuries down the line. If you have particularly tight hip flexors, your body will start to create an anterior pull on the pelvis (anterior pelvic tilt). You can identify an anterior pelvic tilt if your belly protrudes slightly in the front while your butt sticks out in the back (what some people refer to as “duck butt”).
An injury to a ligament is called a sprain, and an injury to muscle or tendon is called a strain. Sprains and strains may be caused by repetitive movements or a single stressful incident. Symptoms and signs include pain and swelling. Though treatment depends upon the extent and location of the injury, rest, ice, compression, and elevation are key elements of treatment.
Using heavy weights: Whether you’re a novice weightlifter or a pro, if you suffer from hip pains you should definitely be putting the kettlebell down! Weight-lifting can place too much stress on your body, especially your knees, lower back and hips. You should be focusing instead on gentle strengthening exercises and stretches in order to support your body as it recovers.
When a muscle contracts, it shortens. Take the biceps for example. Without getting too technical, the biceps are attached at the forearm and shoulder. When your biceps contract, they shorten and bring those two points closer together. When you rest, the muscle returns to its normal length, and the two points move farther away. Constantly contracting your biceps over a long period of time would cause them to get shorter, even at rest.

Sleeping in an awkward position can cause you to be in pain from the moment you wake up. The best sleeping position for lower back pain may be sleeping on your side with your knees drawn up close to your chest (also known as the fetal position). Placing a pillow or two between your legs, while sleeping on your side, helps to reduce stress on your lower back. Sleeping on a too soft mattress can also cause lower back pain. A firmer mattress is best.
Dr. Shiel received a Bachelor of Science degree with honors from the University of Notre Dame. There he was involved in research in radiation biology and received the Huisking Scholarship. After graduating from St. Louis University School of Medicine, he completed his Internal Medicine residency and Rheumatology fellowship at the University of California, Irvine. He is board-certified in Internal Medicine and Rheumatology.
In diagnosing the causes of hip pain, it’s important to understand hip anatomy. The hip is basically a ball-and-socket joint similar to the shoulder joint and the arms. The hip joint is impressive in that it serves two factors, it is a support structure and also very flexible. Because it is a strong support structure, it tends to get injured. Because it’s very flexible, it similarly can be susceptible to injuries.
The hip joint is designed to withstand repeated motion and a fair amount of wear and tear. This ball-and-socket joint—the body’s largest ball-and-socket joint—fits together in a way that allows for fluid movement. While many causes of hip pain can arise from the joint itself, there are numerous structures surrounding the hip that can also be the source of pain.
Work on strengthening all of your core muscles and glutes. These muscles work together to give you balance and stability and to help you move through the activities involved in daily living, as well as exercise and sports. When one set of these muscles is weak or tight, it can cause injury or pain in another, so make sure you pay equal attention to all of them.
From a physical therapist’s perspective, these are excellent exercises for lower back pain (LBP) resulting from muscular tightness or stiff joints. However, LBP can also be caused by bulging (or “herniated”) discs, pinched nerves, and the like. If your LBP worsens (or radiates into your leg) upon attempting these or any other low back exercises, you should seek medical attention. Physical therapists are musculoskeletal experts that are able to properly evaluate and treat your back pain symptoms. And, according to a recently passed law in the state of Michigan, a physician referral is no longer necessary to seek treatment from a physical therapist. So, if you are experiencing LBP that is not improving…#getPT! 
3. Hug it out. Start the supine hip flexor stretch the same as the glute bridge, but keep the right leg relaxed on the floor. Pull shoulder blades down and back to lift hips. Grab the back thigh of the left leg and pull the knee toward the chest. Keep the right leg straight and push its heel into the floor (to feel it in the butt). Hold for 30-45 seconds and switch legs.
The discs are pads that serve as "cushions" between the individual vertebral bodies. They help to minimize the impact of stress forces on the spinal column. Each disc is designed like a jelly donut with a central, softer component (nucleus pulposus) and a surrounding, firm outer ring (annulus fibrosus). The central portion of the disc is capable of rupturing (herniating as in a herniated disc) through the outer ring, causing irritation of adjacent nervous tissue and sciatica as described below. Ligaments are strong fibrous soft tissues that firmly attach bones to bones. Ligaments attach each of the vertebrae to each other and surround each of the discs.
Premkumar et al present evidence that the traditional “red flags” for ominous causes of back pain can be quite misleading. The correlation between red flags and ominous diagnoses is poor, and prone to producing false negatives: that is, no red flags even when there is something more serious than unexplained pain going on. In a survey of almost 10,000 patients “the absence of red flag responses did not meaningfully decrease the likelihood of a red flag diagnosis.“ This is not even remotely a surprise to anyone who paid attention in back pain school, but it’s good to have some harder data on it.
Most low back pain is acute, or short term, and lasts a few days to a few weeks. It tends to resolve on its own with self-care and there is no residual loss of function. The majority of acute low back pain is mechanical in nature, meaning that there is a disruption in the way the components of the back (the spine, muscle, intervertebral discs, and nerves) fit together and move.
5. Feel free as a bird. Open up those hips with yoga’s pigeon pose! Start on all fours with hands below the shoulders and knees below the hips. Bring the right knee forward until it touches the right hand and place the leg flat on the ground across the body (the right foot is now on the left side of the body, parallel to the front of the mat). Drop left leg to the ground, and extend it back with toes turned under. Keep the hips level, inhale, and walk hands forward. Exhale, and fold the torso over, lowering elbows to the floor. Stay in this position for 5-10 breaths before coming back up to switch sides.