Electrodiagnostics are procedures that, in the setting of low back pain, are primarily used to confirm whether a person has lumbar radiculopathy. The procedures include electromyography (EMG), nerve conduction studies (NCS), and evoked potential (EP) studies. EMG assesses the electrical activity in a muscle and can detect if muscle weakness results from a problem with the nerves that control the muscles. Very fine needles are inserted in muscles to measure electrical activity transmitted from the brain or spinal cord to a particular area of the body. NCSs are often performed along with EMG to exclude conditions that can mimic radiculopathy. In NCSs, two sets of electrodes are placed on the skin over the muscles. The first set provides a mild shock to stimulate the nerve that runs to a particular muscle. The second set records the nerve’s electrical signals, and from this information nerve damage that slows conduction of the nerve signal can be detected. EP tests also involve two sets of electrodes—one set to stimulate a sensory nerve, and the other placed on the scalp to record the speed of nerve signal transmissions to the brain.

Vertebroplasty and kyphoplasty are minimally invasive treatments to repair compression fractures of the vertebrae caused by osteoporosis. Vertebroplasty uses three-dimensional imaging to assist in guiding a fine needle through the skin into the vertebral body, the largest part of the vertebrae. A glue-like bone cement is then injected into the vertebral body space, which quickly hardens to stabilize and strengthen the bone and provide pain relief. In kyphoplasty, prior to injecting the bone cement, a special balloon is inserted and gently inflated to restore height to the vertebral structure and reduce spinal deformity.

When I do a deep knee bend like a sumo squat I get a popping in the outside of my left knee. It feels like a big tendon or ligament is slipping per something. It isn’t painful peer se but I’m afraid if I do it a lot it will be. Is that a relatively common symptom for a guy with tight flexors, it bands, etc? Should I just push through it or have it checked out?

How to: Stand tall, feet slightly wider than shoulder-width apart, toes pointed out at 45-degree angles (a). Keep your back straight, knees over toes and your weight in the heels of your feet (b). Engage your glutes and thighs as you lower into a deep squat until thighs parallel to the ground (or as close as you can get them) (c). Powering through your heels, push up to return to starting position (d). Repeat.

A healthy diet is important for a number of reasons when you have lower back pain. First, eating well can help you maintain a healthy weight. Excess weight puts extra strain on your lower back, adding to your pain. Second, a diet that’s high in key nutrients can help promote bone growth and keep your bones strong. These must-have nutrients include:

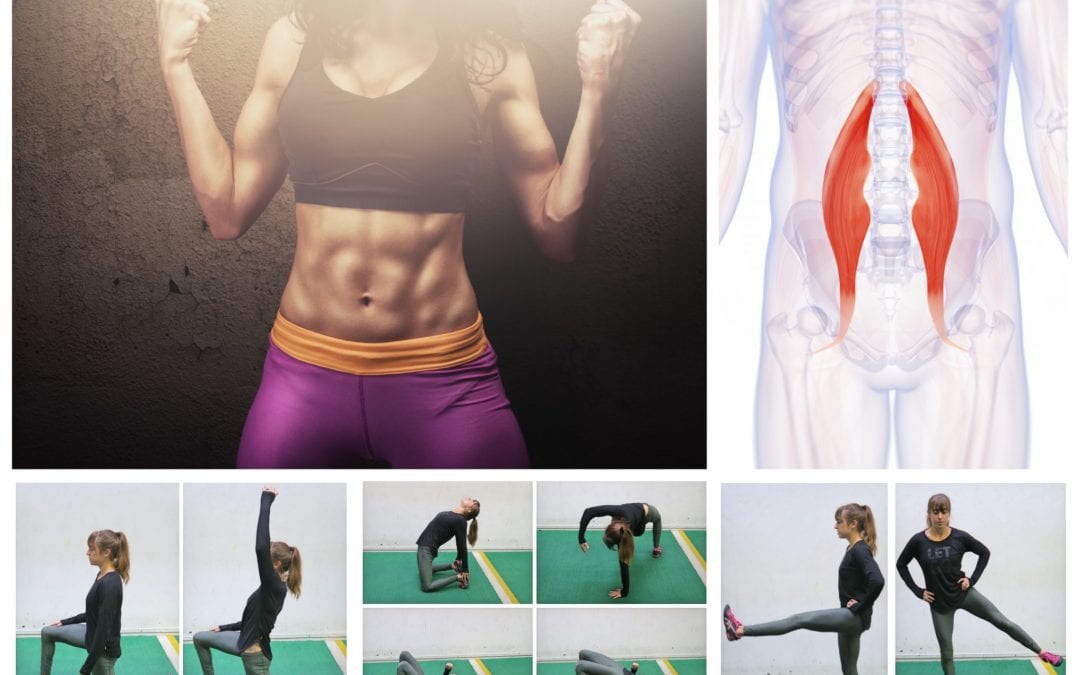
"Lower back pain is the most common musculoskeletal ailment in the U.S., and can often be mitigated by strengthening the core musculature," Blake Dircksen, D.P.T., C.S.C.S., a physical therapist at Bespoke Treatments New York, tells SELF. "The 'core' is a cylinder of abdominal and back muscles that wraps around the body like a corset," Dircksen explains. (The glutes are also considered a part of the core, since they connect to the pelvis and ultimately the back and abdominal muscles.) As with any muscles, by strengthening them, you will increase the amount of weight your lower back can comfortably move, which means it will be better equipped to handle the same stress from your workouts and everyday life without getting as achey.
This Web site provides general educational information on health-related issues and provides access to health-related resources for the convenience of our users. This site and its health-related information and resources are not a substitute for professional medical advice or for the care that patients receive from their physicians or other health care providers.


Avoid stress: Sometimes the worst thing about pain is the stress it can cause. If you aren’t aching all over you can spend most of your time worrying the pain will return or, if you are already in pain, you can start to stress over how it is impacting your life. You really should try to avoid working yourself into a panic though – it really isn’t doing you any good.
Paget's disease of the bone is a condition of unknown cause in which the bone formation is out of synchrony with normal bone remodeling. This condition results in abnormally weakened bone and deformity and can cause localized bone pain, though it often causes no symptoms. Paget's disease is more common in people over the age of 50. Heredity (genetic background) and certain unusual virus infections have been suggested as causes. Thickening of involved bony areas of the lumbar spine can cause the radiating lower extremity pain of sciatica.
Compressive pain is a result of pressure or irritation on the spinal cord, nerves that leave the spine. For example, if an intervertebral disc herniates (usually called a ruptured disc) and pushes into the spinal canal, it can cause problems with the nerve. Usually this pressure or irritation causes pain, numbness, and muscle weakness where the nerve travels.
Meanwhile, it’s extremely common for non-life-threatening low back pain to be alarmingly severe and persistent — to have a loud bark! Your doctor may not appreciate how true this is, and may over-react to all persistent low back pain, even without other red flags. In most cases, you shouldn’t let them scare you. Being “freaked out” about persistent back pain is the real threat: it can make low back pain much worse, and much more likely to last even longer (a tragic irony).

The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed physician should be consulted for diagnosis and treatment of any and all medical conditions. Call 911 for all medical emergencies. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. Copyright 1997-2019, A.D.A.M., Inc. Duplication for commercial use must be authorized in writing by ADAM Health Solutions.
Low back pain has been with humans since at least the Bronze Age. The oldest known surgical treatise – the Edwin Smith Papyrus, dating to about 1500 BCE – describes a diagnostic test and treatment for a vertebral sprain. Hippocrates (c. 460 BCE – c. 370 BCE) was the first to use a term for sciatic pain and low back pain; Galen (active mid to late second century CE) described the concept in some detail. Physicians through the end of the first millennium did not attempt back surgery and recommended watchful waiting. Through the Medieval period, folk medicine practitioners provided treatments for back pain based on the belief that it was caused by spirits.[99]
Neglect your lower body too often and you risk losing mobility — that thing that allows you to plop down on the floor to play with your kids, or get up and out of even the cushiest chair with ease. “A lot of people sit all day, so they’re not necessarily using their glute muscles,” says Daily Burn Fitness/Nutrition Coach Allie Whitesides. “And a lot of people are in the car all the time, so we’re not using our leg muscles much, either.”
Medicine FinderLatest NewsSlip, slap, slop early to save your skinComplementary medicine users have worse cancer survivalVideo: BoredomPut down the tablet; pick up a bookVideo: Lift your mood with some weightsQuicken your step to live longerThis web site is intended for Australian residents and is not a substitute for independent professional advice. Information and interactions contained in this Web site are for information purposes only and are not intended to be used to diagnose, treat, cure or prevent any disease. Further, the accuracy, currency and completeness of the information available on this Web site cannot be guaranteed. Tonic Digital Media Pty Ltd, its affiliates and their respective servants and agents do not accept any liability for any injury, loss or damage incurred by use of or reliance on the information made available via or through myDr whether arising from negligence or otherwise. See Privacy Policy and Disclaimer.2001-2019 myDr.com.au © | All Rights Reserved About UsContact UsDisclaimerPrivacy PolicyAdvertising PolicySitemap
There is a significant overlap of nerve supply to many of the discs, muscles, ligaments, and other spinal structures, and it can be difficult for the brain to accurately sense which is the cause of the pain. For example, a degenerated or torn lumbar disc can feel the same as a pulled muscle – both creating inflammation and painful muscle spasm in the same area. Muscles and ligaments heal rapidly, while a torn disc may or may not. The time course of pain helps determine the cause.
Really great content. I also had some lower back problem but now that I know the source, I will work on it. My counsins also talked to me about this product called Panifix, or "Unlock your hip flexor" which Gives You A Practical, Easy-to-follow Program You Can Use To Instantly Release Your Hip Flexors For More Strength, Better Health And All Day Energy. Proven Swipes And Creatives Here:https://tinyurl.com/yd6nbzfh
The side of the pain on its own doesn’t tell us much, and most of the one-sided sources of pain are viscera that usually cause abdominal pain instead of back pain, or in addition to it. In other words, the only reason to worry about right or left lower back pain is if it is otherwise worrisome: if you have other red flags or significant non-back symptoms.
Bridge: Still lying on your back with your feet flat on floor, lift your hips and torso off the floor into a bridge. Then interlace your hands underneath your hips and press your shoulders and upper arms into the floor, lifting your hips higher. Hold for 10 seconds. Lower yourself slowly back down, rolling down from the top of your spine to your tailbone. Repeat three times.
Pain in the front of the joint—where the leg attaches to the trunk—is typically caused by hip joint problems. You may also feel pain associated with a hip injury in the lower part of your glutes and the top of the back of your thigh. Other symptoms include the inability to move the leg at the hip, inability to put weight on one leg due to pain at the hip, or swelling around the joint. As runners, you may also experience pain in the hipo joint only when running due to a hip injury.
Paget's disease of the bone is a condition of unknown cause in which the bone formation is out of synchrony with normal bone remodeling. This condition results in abnormally weakened bone and deformity and can cause localized bone pain, though it often causes no symptoms. Paget's disease is more common in people over the age of 50. Heredity (genetic background) and certain unusual virus infections have been suggested as causes. Thickening of involved bony areas of the lumbar spine can cause the radiating lower extremity pain of sciatica.
I’m not endorsing or saying these stretches are a miracle cure, but I definitely think they’ve helped. I’ve even started to add a few gentle yoga poses and pilates moves which I could so easily do, back in the day, when I was 63 kilos and participated in the greatest oxymoron ever named … a thing called the Fun Run. If I’m not careful, and I keep stretching away each day, I could end up with a 6 pack and back to my 5′ 7″ instead of 5′ 5″.
How to do it: Loop a resistance band around your ankles and lie on your right side with your right arm extended on the floor, left hand in front of your body for support. Brace your abs in tight, bring your bottom leg slightly in front of your top leg (let the inside of your top foot rest on the ground), and lift your leg up to the ceiling, keeping your hips stacked. Maintain tension on the band at all times and pulse your bottom leg up and down quickly 20 times. Repeat on the other side.
Kneel on your mat with your thighs perpendicular to the floor and tops of your feet facing down. Bring your inner knees together. Slide your feet apart so they are slightly wider than your hips and press the tops of your feet evenly into the mat. Slowly sit down between your feet. Use your hands to turn the top of your thighs inward. Then, lean back onto your forearms and slowly lower torso to floor. Hold for at least 30 seconds.
With the stakes so high, doesn’t it make sense to do all you can to strengthen and protect your hips? Even if you have arthritis in a hip — the reason for 8 in 10 replacements — you may be able to manage pain with exercise. In a 2017 pilot study published in the Journal of Osteoporosis, women 65 and older who exercised three times a week in a supervised 12-week program reduced arthritic hip pain by over 30 percent, with similar gains in strength, and joint range of motion. The four exercises here will fortify the muscles that surround and support your hips, says trainer Robert Linkul, owner of Be Stronger Fitness in Sacramento, Calif. He advises doing these simple moves, two to three sets of five to 10 reps each, three times a week. Compare how you feel after three weeks.
Long periods of inactivity in bed are no longer recommended, as this treatment may actually slow recovery. Spinal manipulation for periods of up to one month has been found to be helpful in some patients who do not have signs of nerve irritation. Future injury is avoided by using back-protection techniques during activities and support devices as needed at home or work.

Dr. Shiel received a Bachelor of Science degree with honors from the University of Notre Dame. There he was involved in research in radiation biology and received the Huisking Scholarship. After graduating from St. Louis University School of Medicine, he completed his Internal Medicine residency and Rheumatology fellowship at the University of California, Irvine. He is board-certified in Internal Medicine and Rheumatology.
There are cases of low back pain that have alarming causes, but it’s rare. Once in a while back pain is a warning sign of cancer, autoimmune disease, infection, or a handful of other scary culprits.7 Over the age of 55, about one in twenty cases turns out to be a fracture, and one in a hundred is more ominous.8 The further you are from 55, the better your odds.

Take a step back and think about where you spend most of your day. If you're a young athlete, you probably spend most of your time at school or maybe work or practice and even a little time at home, if you're lucky. Now think about what position your body is in during those periods. I would bet that you spend most of your day sitting down. You may walk to class or run in practice, but the majority of your day is spent in a seated position.

Cycling: The repetitive movements of cycling can place a strain on your hip joints, not to mention that it can also affect your posture! If you really must cycle, make sure your bike is professionally fitted and that you properly warm up and stretch your hip flexors before getting on your bike. I’d recommend choosing an alternative though, or at least speaking to your doctor first!
Too much sitting is the enemy of stiff or achy hips, says Lisa Woods, a personal trainer and yoga teacher in Eagle, Colorado. The big problem, though, isn’t just the discomfort in the sides of your thighs. It’s the chain of pain that dysfunctional hips can create, including sciatic nerve pain that can start in your lower back and go down the backs of your legs.
Meanwhile, it’s extremely common for non-life-threatening low back pain to be alarmingly severe and persistent — to have a loud bark! Your doctor may not appreciate how true this is, and may over-react to all persistent low back pain, even without other red flags. In most cases, you shouldn’t let them scare you. Being “freaked out” about persistent back pain is the real threat: it can make low back pain much worse, and much more likely to last even longer (a tragic irony).
If most inner-thigh openers feel too easy (and your ankles and knees are injury-free), try Frog Pose. Get down on all fours, with palms on the floor and your knees on blankets or a mat (roll your mat lengthwise, like a tortilla, and place it under your knees for more comfort). Slowly widen your knees until you feel a comfortable stretch in your inner thighs, keeping the inside of each calf and foot in contact with the floor. Make sure to keep your ankles in line with your knees. Lower down to your forearms. Stay here for at least 30 seconds.
Really great content. I also had some lower back problem but now that I know the source, I will work on it. My counsins also talked to me about this product called Panifix, or "Unlock your hip flexor" which Gives You A Practical, Easy-to-follow Program You Can Use To Instantly Release Your Hip Flexors For More Strength, Better Health And All Day Energy. Proven Swipes And Creatives Here:https://tinyurl.com/yd6nbzfh
Low back pain may be classified based on the signs and symptoms. Diffuse pain that does not change in response to particular movements, and is localized to the lower back without radiating beyond the buttocks, is classified as nonspecific, the most common classification.[5] Pain that radiates down the leg below the knee, is located on one side (in the case of disc herniation), or is on both sides (in spinal stenosis), and changes in severity in response to certain positions or maneuvers is radicular, making up 7% of cases.[5] Pain that is accompanied by red flags such as trauma, fever, a history of cancer or significant muscle weakness may indicate a more serious underlying problem and is classified as needing urgent or specialized attention.[5]

The treatment of hip pain depends on the precise cause of the pain. Treatments can include rest, non-weight-bearing, cold application, and anti-inflammatory medications. For local inflammation, sometimes injection of cortisone medication (steroids) is used to quiet the inflammation. If infection is present, antibiotics are used. Fractures can require treatment with surgical repairs, including pinning, plates and screws, and total joint replacement. For severe arthritis, total joint replacement is performed when possible.
If certain activities or overuse are causing hip pain, stop those that aggravate the discomfort and talk to your doctor. Excess weight can put pressure on the hip joint, so losing the pounds can provide relief and help you avoid further problems. Some causes of hip pain, such as fractures or hernias, may need surgical repairs. If your hip pain persists, talk to your doctor about the possible causes and treatments.

Chronic back pain is defined as pain that persists for 12 weeks or longer, even after an initial injury or underlying cause of acute low back pain has been treated. About 20 percent of people affected by acute low back pain develop chronic low back pain with persistent symptoms at one year. In some cases, treatment successfully relieves chronic low back pain, but in other cases pain persists despite medical and surgical treatment.
3. Tendinitis and bursitis Many tendons around the hip connect the muscles to the joint. These tendons can easily become inflamed if you overuse them or participate in strenuous activities. One of the most common causes of tendinitis at the hip joint, especially in runners, is iliotibial band syndrome — the iliotibial band is the thick span of tissue that runs from the outer rim of your pelvis to the outside of your knee.
When I do a deep knee bend like a sumo squat I get a popping in the outside of my left knee. It feels like a big tendon or ligament is slipping per something. It isn’t painful peer se but I’m afraid if I do it a lot it will be. Is that a relatively common symptom for a guy with tight flexors, it bands, etc? Should I just push through it or have it checked out?
Why is back pain still a huge problem? Maybe this: “It is extremely difficult to alter the potentially disabling belief among the lay public that low back pain has a structural mechanical cause. An important reason for this is that this belief continues to be regularly reinforced by the conditions of care of a range of ‘hands-on’ providers, for whom idiosyncratic variations of that view are fundamental to their professional existence.”
Bone scans are used to detect and monitor infection, fracture, or disorders in the bone. A small amount of radioactive material is injected into the bloodstream and will collect in the bones, particularly in areas with some abnormality. Scanner-generated images can be used to identify specific areas of irregular bone metabolism or abnormal blood flow, as well as to measure levels of joint disease.

Parts of the pain sensation and processing system may not function properly; creating the feeling of pain when no outside cause exists, signaling too much pain from a particular cause, or signaling pain from a normally non-painful event. Additionally, the pain modulation mechanisms may not function properly. These phenomena are involved in chronic pain.[12]
Magnetic resonance imaging (MRI) uses a magnetic force instead of radiation to create a computer-generated image. Unlike x-ray, which shows only bony structures, MRI scans also produce images of soft tissues such as muscles, ligaments, tendons, and blood vessels. An MRI may be ordered if a problem such as infection, tumor, inflammation, disc herniation or rupture, or pressure on a nerve is suspected. MRI is a noninvasive way to identify a condition requiring prompt surgical treatment. However, in most instances, unless there are “red flags” in the history or physical exam, an MRI scan is not necessary during the early phases of low back pain.
Avoiding injury to the low back is a method of preventing low back pain. Additionally, conditioning exercise programs designed to strengthen the lumbar area and adjacent tissues can help to minimize risk of injury to the low back. Specific programs to relieve and prevent back pain can be designed with the help of physical therapists and other treating health-care professionals.
Some of these red flags are much less red than others, especially depending on the circumstances. For instance, “weight loss” is common and often the sign of successful diet! (Well, at least temporarily successful, anyway. 😃) Obviously, if you know of a harmless reason why you have a red flag symptom, it isn’t really a red flag (duh!). But every single actual red flag — in combination with severe low back pain that’s been going on for several weeks — is definitely a good reason to get yourself checked out.