The management of low back pain often includes medications for the duration that they are beneficial. With the first episode of low back pain the hope is a complete cure; however, if the problem becomes chronic, the goals may change to pain management and the recovery of as much function as possible. As pain medications are only somewhat effective, expectations regarding their benefit may differ from reality, and this can lead to decreased satisfaction.[13]
Really a great content. Let me tell you first about hip flexor it is the engine through which our body moves. They control balance, our ability to sit, stand, twist, reach, bend, walk and step. One of my patient also suffering from same problem but due to lack of money he was unable to afford a treatment. So i recommend him a program to unlock hip flexor. If anyone wants they can check it out here ;- https://tinyurl.com/y8yaqs2s Report
Initial management with non–medication based treatments is recommended.[6] NSAIDs are recommended if these are not sufficiently effective.[6] Normal activity should be continued as much as the pain allows.[2] Medications are recommended for the duration that they are helpful.[13] A number of other options are available for those who do not improve with usual treatment. Opioids may be useful if simple pain medications are not enough, but they are not generally recommended due to side effects.[4][13] Surgery may be beneficial for those with disc-related chronic pain and disability or spinal stenosis.[14][15] No clear benefit has been found for other cases of non-specific low back pain.[14] Low back pain often affects mood, which may be improved by counseling or antidepressants.[13][16] Additionally, there are many alternative medicine therapies, including the Alexander technique and herbal remedies, but there is not enough evidence to recommend them confidently.[17] The evidence for chiropractic care[18] and spinal manipulation is mixed.[17][19][20][21] 
Premkumar et al present evidence that the traditional “red flags” for ominous causes of back pain can be quite misleading. The correlation between red flags and ominous diagnoses is poor, and prone to producing false negatives: that is, no red flags even when there is something more serious than unexplained pain going on. In a survey of almost 10,000 patients “the absence of red flag responses did not meaningfully decrease the likelihood of a red flag diagnosis.“ This is not even remotely a surprise to anyone who paid attention in back pain school, but it’s good to have some harder data on it.
The multifidus muscles run up and down along the back of the spine, and are important for keeping the spine straight and stable during many common movements such as sitting, walking and lifting.[12] A problem with these muscles is often found in someone with chronic low back pain, because the back pain causes the person to use the back muscles improperly in trying to avoid the pain.[31] The problem with the multifidus muscles continues even after the pain goes away, and is probably an important reason why the pain comes back.[31] Teaching people with chronic low back pain how to use these muscles is recommended as part of a recovery program.[31]
Neglect your lower body too often and you risk losing mobility — that thing that allows you to plop down on the floor to play with your kids, or get up and out of even the cushiest chair with ease. “A lot of people sit all day, so they’re not necessarily using their glute muscles,” says Daily Burn Fitness/Nutrition Coach Allie Whitesides. “And a lot of people are in the car all the time, so we’re not using our leg muscles much, either.”
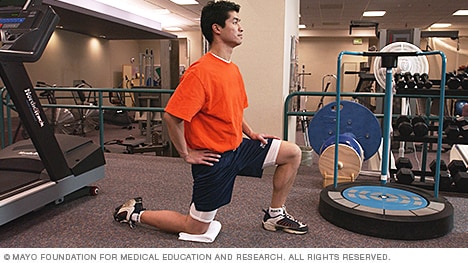
Stretching the hip muscles that sit on top of the bursae, part of the lining in your hip joint, can give you some relief from bursitis pain. Kneel on the leg that's giving you the pain, holding on to something sturdy for balance. Tilt your pelvis forward, tightening your gluteus muscles (the muscles in your buttocks). Then lean away from the side of your hip that hurts, for instance to the left if you're kneeling on your right knee. You should feel a stretch from the top of your hip bone down the side of your leg to your knee, Humphrey says. Hold the stretch for 30 seconds and repeat once or twice.
Running: Running may be good for boosting your cardiovascular health but it can be very strenuous if you have hip pain. The impact can upset your hip joints so instead focus on other forms of exercise. Walking is still a good option for hip pain if you really feel like working out in the great outdoors or you could instead try some strengthening exercises from the comfort of your own home.
If you’re worried you’re headed toward a surgeon’s office, there might be hope. According to the Arthritis Foundation, the best way to avoid hip replacement surgery is to get active in an exercise program. In a study, people who participated in an exercise program for 12 weeks were 44 percent less likely to need joint-replacement surgery six years later than those who did not exercise.

^ Jump up to: a b c d e f Qaseem, A; Wilt, TJ; McLean, RM; Forciea, MA; Clinical Guidelines Committee of the American College of, Physicians. (4 April 2017). "Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians". Annals of Internal Medicine. 166 (7): 514–530. doi:10.7326/M16-2367. PMID 28192789.
Lie on your back with your knees bent and feet flat on the floor. Place left ankle right below right knee, creating a “four” shape with left leg. Thread left arm through the opening you created with left leg and clasp hands behind right knee. Lift right foot off floor and pull right knee toward chest, flexing left foot. Hold for 30 seconds, then repeat on opposite side.
Following any period of prolonged inactivity, a regimen of low-impact exercises is advised. Speed walking, swimming, or stationary bike riding 30 minutes daily can increase muscle strength and flexibility. Yoga also can help stretch and strengthen muscles and improve posture. Consult a physician for a list of low-impact, age-appropriate exercises that are specifically targeted to strengthening lower back and abdominal muscles.
Physician specialties that evaluate and treat low back pain range from generalists to subspecialists.These specialties include emergency medicine physicians, general medicine, family medicine, internal medicine, gynecology, spine surgeons (orthopaedics and neurosurgery), rheumatology, pain management, and physiatry. Other health care providers for low back pain include physical therapists, chiropractors, massage therapists, psychologists, and acupuncturists.

Men and women are equally affected by low back pain, which can range in intensity from a dull, constant ache to a sudden, sharp sensation that leaves the person incapacitated. Pain can begin abruptly as a result of an accident or by lifting something heavy, or it can develop over time due to age-related changes of the spine. Sedentary lifestyles also can set the stage for low back pain, especially when a weekday routine of getting too little exercise is punctuated by strenuous weekend workout.
Pregnancy symptoms can vary from woman to woman, and not all women experience the same symptoms. When women do experience pregnancy symptoms they may include symptoms include missed menstrual period, mood changes, headaches, lower back pain, fatigue, nausea, breast tenderness, and heartburn. Signs and symptoms in late pregnancy include leg swelling and shortness of breath. Options for relief of pregnancy symptoms include exercise, diet, and other lifestyle changes.

Bony encroachment: Any condition that results in movement or growth of the vertebrae of the lumbar spine can limit the space (encroachment) for the adjacent spinal cord and nerves. Causes of bony encroachment of the spinal nerves include foraminal narrowing (narrowing of the portal through which the spinal nerve passes from the spinal column, out of the spinal canal to the body, commonly as a result of arthritis), spondylolisthesis (slippage of one vertebra relative to another), and spinal stenosis (compression of the nerve roots or spinal cord by bony spurs or other soft tissues in the spinal canal). Spinal-nerve compression in these conditions can lead to sciatica pain that radiates down the lower extremities. Spinal stenosis can cause lower-extremity pains that worsen with walking and are relieved by resting (mimicking the pains of poor circulation). Treatment of these afflictions varies, depending on their severity, and ranges from rest and exercises to epidural cortisone injections and surgical decompression by removing the bone that is compressing the nervous tissue.
Lie on your back with your knees bent and your feet flat on the floor. Tighten your buttocks and lift your hips off the floor. Tighten your abdominal muscles and lift one foot a couple of inches off the floor. Then put it down and lift the other foot a couple of inches, all while remembering to breathe. “It’s like taking alternate steps,” Pariser says. Work up to doing 30 steps at a time.
Treatment options include physical therapy, back exercises, weight reduction, steroid injections (epidural steroids), nonsteroidal anti-inflammatory medications, rehabilitation and limited activity. All of these treatment options are aimed at relieving the inflammation in the back and irritation of nerve roots. Physicians usually recommend four to six weeks of conservative therapy before considering surgery.

Compressive pain is a result of pressure or irritation on the spinal cord, nerves that leave the spine. For example, if an intervertebral disc herniates (usually called a ruptured disc) and pushes into the spinal canal, it can cause problems with the nerve. Usually this pressure or irritation causes pain, numbness, and muscle weakness where the nerve travels.
An injury to a ligament is called a sprain, and an injury to muscle or tendon is called a strain. Sprains and strains may be caused by repetitive movements or a single stressful incident. Symptoms and signs include pain and swelling. Though treatment depends upon the extent and location of the injury, rest, ice, compression, and elevation are key elements of treatment.
Icing a joint that’s inflamed because of arthritis or bursitis can lower inflammation and help with hip pain. “If it’s very painful, I sometimes tell patients to ice four or five times daily for about 10 to 15 minutes,” says Amy Humphrey, DPT, a physical therapist at Body Dynamics, Inc. in Arlington, Va. Use an ice pack, wrap a towel around it, and put it where you feel the pain.
Place a mini band around your ankles and spread your feet about shoulder-width apart. Keeping your legs relatively straight (you want the motion to come from your hips) and toes pointing forward, walk forward 10 steps, then backward 10 steps. Take a short break and then walk to the right 10 steps, then to the left 10 steps. Again, focus on keeping your legs straight and toes pointing forward.
Compressive pain is a result of pressure or irritation on the spinal cord, nerves that leave the spine. For example, if an intervertebral disc herniates (usually called a ruptured disc) and pushes into the spinal canal, it can cause problems with the nerve. Usually this pressure or irritation causes pain, numbness, and muscle weakness where the nerve travels.
Pain is generally an unpleasant feeling in response to an event that either damages or can potentially damage the body's tissues. There are four main steps in the process of feeling pain: transduction, transmission, perception, and modulation.[12] The nerve cells that detect pain have cell bodies located in the dorsal root ganglia and fibers that transmit these signals to the spinal cord.[33] The process of pain sensation starts when the pain-causing event triggers the endings of appropriate sensory nerve cells. This type of cell converts the event into an electrical signal by transduction. Several different types of nerve fibers carry out the transmission of the electrical signal from the transducing cell to the posterior horn of spinal cord, from there to the brain stem, and then from the brain stem to the various parts of the brain such as the thalamus and the limbic system. In the brain, the pain signals are processed and given context in the process of pain perception. Through modulation, the brain can modify the sending of further nerve impulses by decreasing or increasing the release of neurotransmitters.[12]
To understand various causes of low back pain, it is important to appreciate the normal design (anatomy) of the tissues of this area of the body. Important structures of the low back that can be related to symptoms in this region include the bony lumbar spine (vertebrae, singular = vertebra), discs between the vertebrae, ligaments around the spine and discs, spinal cord and nerves, muscles of the low back, internal organs of the pelvis and abdomen, and the skin covering the lumbar area.
Talmage, J; Belcourt, R; Galper, J; et al. (2011). "Low back disorders". In Kurt T. Hegmann. Occupational medicine practice guidelines : evaluation and management of common health problems and functional recovery in workers (3rd ed.). Elk Grove Village, IL: American College of Occupational and Environmental Medicine. pp. 336, 373, 376–377. ISBN 978-0615452272.
Located deep in the front of the hip and connecting the leg, pelvis, and abdomen, the hip flexors— surprise, surprise— flex the hip. But despite being some of the most powerful muscles in our bodies (with a clearly important role), it’s easy to neglect our poor hip flexors— often without even knowing it. It turns out just working at a desk all day (guilty!) can really weaken hip flexors since they tend to shorten up while in a seated position. This tightness disrupts good posture and is a common cause of lower back pain. Weakened hip flexors can also increase the risk of foot, ankle, and knee injuries (especially among runners) Hip muscle weakness and overuse injuries in recreational runners. Niemuth, P.E., Johnson, R.J., Myers, M.J., et al. Rocky Mountain University of Health Professions, Provo, VT. Clinical Journal of Sport Medicine, 2005 Jan; 15 (1): 14-21.. So be sure to get up, stand up every hour or so! And giving the hip flexors some extra attention is not just about injury prevention. Adding power to workouts, working toward greater flexibility, and getting speedier while running is also, as they say, all in the hips The effect of walking speed on muscle function and mechanical energetics. Neptune, R.R., Sasaki, K., and Kautz, S.A. Department of Mechanical Engineering, The University of Texas, Austin, TX. Gait & Posture, 2008 Jul; 28 (1): 135-43..

Iliopsoas syndrome, which is also called psoas syndrome or iliopsoas tendonitis, occurs when the iliopsoas muscles are injured. Lower back pain is the most common symptom; however, pain can also occur in the hip, thigh, or leg. The iliopsoas bursa, which is a fluid-filled sac located on the inside of the hip that reduces rubbing and friction, is also likely to become inflamed due to the proximity of the two structures. When this happens, the inflamed bursae will make it difficult to move.


