Imaging is indicated when there are red flags, ongoing neurological symptoms that do not resolve, or ongoing or worsening pain.[5] In particular, early use of imaging (either MRI or CT) is recommended for suspected cancer, infection, or cauda equina syndrome.[5] MRI is slightly better than CT for identifying disc disease; the two technologies are equally useful for diagnosing spinal stenosis.[5] Only a few physical diagnostic tests are helpful.[5] The straight leg raise test is almost always positive in those with disc herniation.[5] Lumbar provocative discography may be useful to identify a specific disc causing pain in those with chronic high levels of low back pain.[41] Similarly, therapeutic procedures such as nerve blocks can be used to determine a specific source of pain.[5] Some evidence supports the use of facet joint injections, transforminal epidural injections and sacroilliac injections as diagnostic tests.[5] Most other physical tests, such as evaluating for scoliosis, muscle weakness or wasting, and impaired reflexes, are of little use.[5]
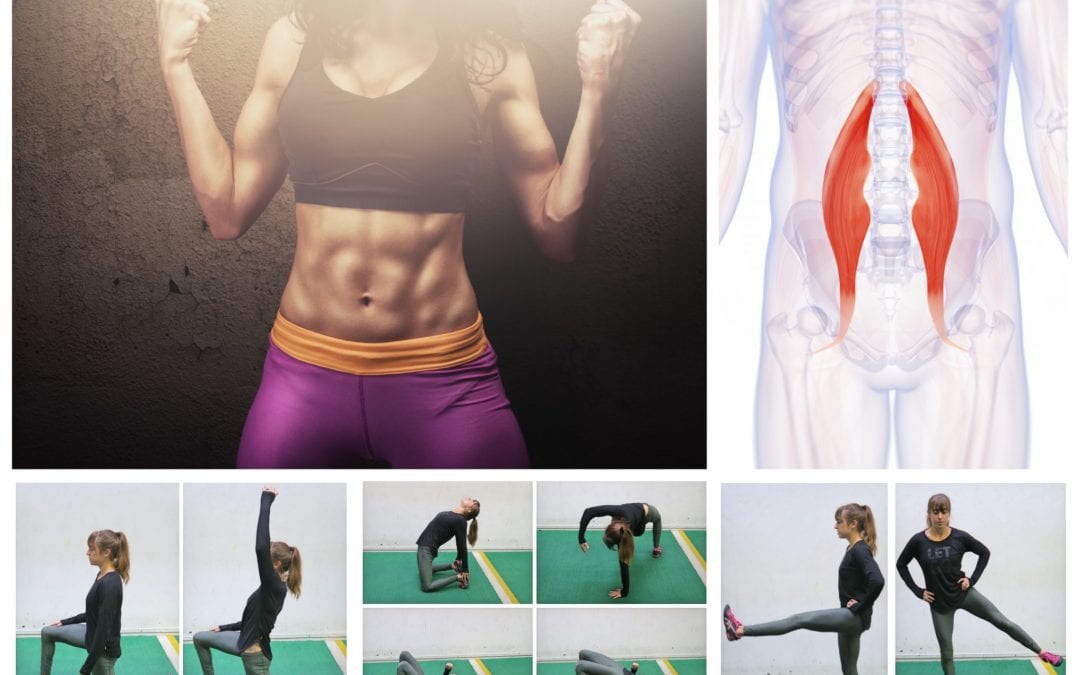
How to: Position yourself on your hands and knees, in tabletop position. Engage your abs engaged by pulling your belly button in towards your spine (a). Keeping your hips pointed towards the ground and leg bent to a 90-degree angle, raise your left knee out to the side as high as you can (b). Pause at the top, then return to starting position (c). Repeat, then switch legs.

This standard recommendation reinforces the alarming idea that low back pain that lasts longer than a few weeks is Really Bad News. It’s not. It’s a clue. It’s a reason for concern and alertness. But many cases of low back pain that last for 6 weeks will still go away. Once again, see the 2009 research published in the British Medical Journal, which showed that more than 30% of patients with “new” chronic low back pain will still recover without treatment. BACK TO TEXT
Prior to doing this, warm up to avoid overstretching a cold muscle. Great ways to warm up include jumping jacks, skipping, side-stepping, running in place, or any dynamic movements that mimic whatever sport you do. Given that this targets the lower half of your body, it's best to choose movements that will make the muscles in the groin and inner thigh areas warm and pliable.
Compressive pain is a result of pressure or irritation on the spinal cord, nerves that leave the spine. For example, if an intervertebral disc herniates (usually called a ruptured disc) and pushes into the spinal canal, it can cause problems with the nerve. Usually this pressure or irritation causes pain, numbness, and muscle weakness where the nerve travels.
Lumbar radiculopathy: Lumbar radiculopathy is nerve irritation that is caused by damage to the discs between the vertebrae. Damage to the disc occurs because of degeneration ("wear and tear") of the outer ring of the disc, traumatic injury, or both. As a result, the central softer portion of the disc can rupture (herniate) through the outer ring of the disc and abut the spinal cord or its nerves as they exit the bony spinal column. This rupture is what causes the commonly recognized "sciatica" pain of a herniated disc that shoots from the low back and buttock down the leg. Sciatica can be preceded by a history of localized low-back aching or it can follow a "popping" sensation and be accompanied by numbness and tingling. The pain commonly increases with movements at the waist and can increase with coughing or sneezing. In more severe instances, sciatica can be accompanied by incontinence of the bladder and/or bowels. The sciatica of lumbar radiculopathy typically affects only one side of the body, such as the left side or right side, and not both. Lumbar radiculopathy is suspected based on the above symptoms. Increased radiating pain when the lower extremity is lifted supports the diagnosis. Nerve testing (EMG/electromyogramspina bifida

Analgesic medications are those specifically designed to relieve pain. They include OTC acetaminophen and aspirin, as well as prescription opioids such as codeine, oxycodone, hydrocodone, and morphine. Opioids should be used only for a short period of time and under a physician’s supervision. People can develop a tolerance to opioids and require increasingly higher dosages to achieve the same effect. Opioids can also be addictive. Their side effects can include drowsiness, constipation, decreased reaction time, and impaired judgment. Some specialists are concerned that chronic use of opioids is detrimental to people with back pain because they can aggravate depression, leading to a worsening of the pain.
Apply the above concept to your hips. When you sit, your hips are in a "flexed" position. Therefore, the muscles that flex your hips are in a shortened state. You probably spend at least a third of your day sitting down. Think about how much time those hip flexor muscles stay shortened. A lot. Over time, they become tighter and tighter until you look like the old man in the picture. So unless you want to look like that, perform the stretches shown below.
Some of these red flags are much less red than others, especially depending on the circumstances. For instance, “weight loss” is common and often the sign of successful diet! (Well, at least temporarily successful, anyway. 😃) Obviously, if you know of a harmless reason why you have a red flag symptom, it isn’t really a red flag (duh!). But every single actual red flag — in combination with severe low back pain that’s been going on for several weeks — is definitely a good reason to get yourself checked out.