The problem is that these muscles aren't designed to be prime movers—they're designed to support the action of the glutes. Inability of activating the glutes can result in low back pain (low back muscles compensating), hamstring strains (overacting hamstrings), hip pain (resulting from hamstring-dominant hip extension) and knee pain (poor glute medius strength).
For the 31 million Americans who suffer from daily back pain, relief can be hard to find. In fact, back pain is the single leading cause of disability worldwide and the second most common reason for visits to the doctor. While it can be caused by many different things—extended periods of sitting or standing at work, bad posture, stress, an overly-strenuous workout or helping a friend move, to mention a few—once back pain hits, it can stick around for a long time. Your gut instinct might be to stay frozen until it goes away, but the best thing for your back is to keep it moving with gentle stretches. In fact, a regular routine of a few quick exercises can help you reduce your back pain without a trip to the doctor. Try to do the following exercises every morning and again at night.
The only activity performed on a regular basis that fully extends the hip is walking and running. Hence as activity levels decrease so does the ability to extend the hip. This results in compensatory pelvic tilting and lumbar extension, with a reduction in the ability to accommodate uneven ground, negotiate obstacles, or attempt to change walking speed quickly. The compensatory pelvic tilt that accompanies tight hip flexors also predisposes the individual to postural problems and back pain. Hip stretches done on a regular basis can help you maintain extension range of motion and thereby improve function.
^ Jump up to: a b c Furlan AD, Yazdi F, Tsertsvadze A, Gross A, Van Tulder M, Santaguida L, Gagnier J, Ammendolia C, Dryden T, Doucette S, Skidmore B, Daniel R, Ostermann T, Tsouros S (2012). "A systematic review and meta-analysis of efficacy, cost-effectiveness, and safety of selected complementary and alternative medicine for neck and low-back pain". Evidence-Based Complementary and Alternative Medicine. 2012: 1–61. doi:10.1155/2012/953139. PMC 3236015. PMID 22203884.
The presence of certain signs, termed red flags, indicate the need for further testing to look for more serious underlying problems, which may require immediate or specific treatment.[5][36] The presence of a red flag does not mean that there is a significant problem. It is only suggestive,[37][38] and most people with red flags have no serious underlying problem.[3][1] If no red flags are present, performing diagnostic imaging or laboratory testing in the first four weeks after the start of the symptoms has not been shown to be useful.[5]

Cat-cow: Start on all fours, with palms and knees on the ground. Slowly arch your back, tilt your butt up and look up at the ceiling so you make a C curve with your torso. Return to the neutral starting position, then tilt your pelvis down and gaze at the floor near your feet, so your body reverses the C curve the other way. Return to neutral and repeat the series three times.
Great exercises and stretches that can be easily done throughout the day to strengthen and loosen my hip flexors. i have very tight hip flexors so it's very helpful for me knowing these exercises and stretches. For those that want more info about exercises and stretches for hip flexors, i recommend the "unlock your hip flexors". It is a program that will show you many more exercises and stretches you can do. So check it out here
The treatment of lumbar strain consists of resting the back (to avoid reinjury), medications to relieve pain and muscle spasm, local heat applications, massage, and eventual (after the acute episode resolves) reconditioning exercises to strengthen the low back and abdominal muscles. Initial treatment at home might include heat application, acetaminophen (Tylenol) or ibuprofen (Advil, Motrin), and avoiding reinjury and heavy lifting. Prescription medications that are sometimes used for acute low back pain include anti-inflammatory medications, such as sulindac (Clinoril), naproxen (Naprosyn), and ketorolac (Toradol) by injection or by mouth, muscle relaxants, such as carisoprodol (Soma), cyclobenzaprine (Flexeril), methocarbamol (Robaxin), and metaxalone (Skelaxin), as well as analgesics, such as tramadol (Ultram).

Foraminotomy is an operation that “cleans out” or enlarges the bony hole (foramen) where a nerve root exits the spinal canal. Bulging discs or joints thickened with age can cause narrowing of the space through which the spinal nerve exits and can press on the nerve, resulting in pain, numbness, and weakness in an arm or leg. Small pieces of bone over the nerve are removed through a small slit, allowing the surgeon to cut away the blockage and relieve pressure on the nerve.
For example, your quadriceps muscles are a group of four that are located at the front of the thigh; one of the group members, the rectus femoris flexes the hip, which brings your lower extremity (thigh, lower leg, and foot) forward, in front of you. On the other hand, your hamstring muscles are located at the back of the thigh. When they contract, they extend the lower extremity, bringing it behind you.

Icing a joint that’s inflamed because of arthritis or bursitis can lower inflammation and help with hip pain. “If it’s very painful, I sometimes tell patients to ice four or five times daily for about 10 to 15 minutes,” says Amy Humphrey, DPT, a physical therapist at Body Dynamics, Inc. in Arlington, Va. Use an ice pack, wrap a towel around it, and put it where you feel the pain.
The main work of your hip flexors is to bring your knee toward your chest and to bend at the waist. Symptoms associated with a hip flexor strain can range from mild to severe and can impact your mobility. If you don’t rest and seek treatment, your hip flexor strain symptoms could get worse. But there are many at-home activities and remedies that can help reduce hip flexor strain symptoms.
The hip joint is designed to withstand a fair amount of wear and tear, but it’s not indestructible. For example, when you walk, a cushion of cartilage helps prevent friction as the hip bone moves in its socket. With age and use, this cartilage can wear down or become damaged, or the hip bone itself can be fractured during a fall. In fact, more than 300,000 adults over 65 are hospitalized for hip fractures each year, according to the Agency for Healthcare Research and Quality.


For example, your quadriceps muscles are a group of four that are located at the front of the thigh; one of the group members, the rectus femoris flexes the hip, which brings your lower extremity (thigh, lower leg, and foot) forward, in front of you. On the other hand, your hamstring muscles are located at the back of the thigh. When they contract, they extend the lower extremity, bringing it behind you.
“Red flags” are signs or symptoms that something medically ominous may be going on. Red flags are not reliable, and their presence is not a diagnosis. When you have some red flags, it only indicates a need to look more closely. Sometimes red flags are missing there really is something serious going on … and sometimes they are a false alarm.18 Check off all that apply … hopefully none or few or only the least alarming of them!
Lay on your back on your mat and pull your knees to your chest. Place your hands on the inside arches of your feet and open your knees wider than shoulder-width apart. Keeping your back pressed into the mat as much as possible, press your feet into hands while pulling down on feet, creating resistance. Breathe deeply and hold for at least 30 seconds.

The side of the pain on its own doesn’t tell us much, and most of the one-sided sources of pain are viscera that usually cause abdominal pain instead of back pain, or in addition to it. In other words, the only reason to worry about right or left lower back pain is if it is otherwise worrisome: if you have other red flags or significant non-back symptoms.
2016 — More editing, more! Added some better information about pain being a poor indicator, and the role of myofascial trigger points. This article has become extremely busy in the last couple months — about 4,000 readers per day, as described here — so I am really polishing it and making sure that it’s the best possible answer to people’s fears about back pain.

Our Keep-It™ guarantee is valid for the first-time purchase of a formula, and redeemable up to three months (90 days) after the purchase date. Multiple bottles, foods, apparel and gear do not fall under this guarantee, however, they may be applicable for return. Fitness equipment, personal care products, knowledge purchases, and DVDs are not eligible for return or refund. For more information and a full list of products that qualify, visit our Keep-It™ page. Further details can be found on our Refund Policy support page.
There is a significant overlap of nerve supply to many of the discs, muscles, ligaments, and other spinal structures, and it can be difficult for the brain to accurately sense which is the cause of the pain. For example, a degenerated or torn lumbar disc can feel the same as a pulled muscle – both creating inflammation and painful muscle spasm in the same area. Muscles and ligaments heal rapidly, while a torn disc may or may not. The time course of pain helps determine the cause.
One of the biggest dangers to your health is constantly sitting for long periods of time which can cause physical and emotional damage. 10 key moves that will help loosen your hip flexor and unlock the power within your body. There is an easy to follow program to unlocking your hip flexors that will strengthen your body, improve your health, and have an all day energy..... https://bit.ly/2HYTPrJ Report
Paget's disease of the bone is a condition of unknown cause in which the bone formation is out of synchrony with normal bone remodeling. This condition results in abnormally weakened bone and deformity and can cause localized bone pain, though it often causes no symptoms. Paget's disease is more common in people over the age of 50. Heredity (genetic background) and certain unusual virus infections have been suggested as causes. Thickening of involved bony areas of the lumbar spine can cause the radiating lower extremity pain of sciatica.
Your hip labrum is a band of cartilage-like tissue that courses around the outer rim of your hip socket. This labrum helps to support the joint and deepen the socket. Sometimes overuse or an injury to your hip can cause a tear in your labrum. A hip labrum tear may result in a condition called femoroacetabular impingement (FAI). When this happens, hip pain may result, and exercises to stretch and stabilize your hip may be performed.
^ Jump up to: a b c d e f Qaseem, A; Wilt, TJ; McLean, RM; Forciea, MA; Clinical Guidelines Committee of the American College of, Physicians. (4 April 2017). "Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians". Annals of Internal Medicine. 166 (7): 514–530. doi:10.7326/M16-2367. PMID 28192789.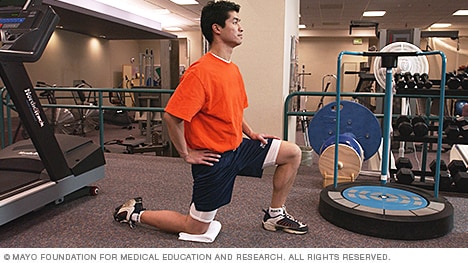
In addition to these exercises, there are simple things you can do every day to help reduce your risk of hip flexor pain. If you sit at a desk for long periods of time, try to get up and move around every hour or so. Warm up properly before any physical activity, and stretch regularly at the end of each workout. Your hips will thank you for it!
Treatment for greater trochanteric bursitis includes stretching and strengthening your IT band, hip abductors, and gluteal muscles, all while avoiding running on banked surfaces. Applying ice to the painful area for 15 minutes, three to four times per day can help, too. A cortisone injection may be beneficial if your injury is severe. Worsening pain should raise suspicion for a stress fracture, in which case you should see your doctor right away.
Place a mini band around your ankles and spread your feet about shoulder-width apart. Keeping your legs relatively straight (you want the motion to come from your hips) and toes pointing forward, walk forward 10 steps, then backward 10 steps. Take a short break and then walk to the right 10 steps, then to the left 10 steps. Again, focus on keeping your legs straight and toes pointing forward.
Emerging technologies such as X-rays gave physicians new diagnostic tools, revealing the intervertebral disc as a source for back pain in some cases. In 1938, orthopedic surgeon Joseph S. Barr reported on cases of disc-related sciatica improved or cured with back surgery.[100] As a result of this work, in the 1940s, the vertebral disc model of low back pain took over,[99] dominating the literature through the 1980s, aiding further by the rise of new imaging technologies such as CT and MRI.[100] The discussion subsided as research showed disc problems to be a relatively uncommon cause of the pain. Since then, physicians have come to realize that it is unlikely that a specific cause for low back pain can be identified in many cases and question the need to find one at all as most of the time symptoms resolve within 6 to 12 weeks regardless of treatment.[99]
Knowing the exact source of your hip pain can provide you with peace of mind—but receiving the right treatment is even better. Let Dr. Hamilton provide you with both peace of mind and relief from your symptoms. Schedule an appointment with Dr. Hamilton today. For your convenience, he is available at Beacon East, Beacon West, or Summit Woods in Ohio as well as Beacon’s Northern Kentucky location.
You may hear a clicking noise when you move your hip, but that sound is not necessarily a hip flexor issue. Siegrist says the clicking isn't generally the hip flexor alone and often comes from a moving part, like the joint. "Maybe there is a loose body in the joint or loose cartilage at the edge of the hip joint that is mechanically getting irritated,” she says.
NINDS-funded studies are contributing to a better understanding of why some people with acute low back pain recover fully while others go on to develop chronic low back pain. Brain imaging studies suggest that people with chronic low back pain have changes in brain structure and function. In one study, people with subacute back pain were followed for one year. Researchers found that certain patterns of functional connectivity across brain networks correlated with the likelihood of pain becoming chronic. The findings suggest that such patterns may help predict who is most likely to transition from subacute to chronic back pain. Other research seeks to determine the role of brain circuits important for emotional and motivational learning and memory in this transition, in order to identify new preventive interventions.
Everything you need to know about osteoarthritis Osteoarthritis is a potentially painful condition that leads to inflammation, loss of cartilage, and bone damage. Read our article to find out how it happens and what treatments can help. Also, see a fully interactive 3-D model that you can explore to look inside a joint when signs of osteoarthritis begin to appear. Read now
Bleeding in the pelvis is rare without significant trauma and is usually seen in patients who are taking blood-thinning medications, such as warfarin (Coumadin). In these patients, a rapid-onset sciatica pain can be a sign of bleeding in the back of the pelvis and abdomen that is compressing the spinal nerves as they exit to the lower extremities. Infection of the pelvis is infrequent but can be a complication of conditions such as diverticulosis, Crohn's disease, ulcerative colitis, pelvic inflammatory disease with infection of the Fallopian tubes or uterus, and even appendicitis. Pelvic infection is a serious complication of these conditions and is often associated with fever, lowering of blood pressure, and a life-threatening state.
Some of these red flags are much less red than others, especially depending on the circumstances. For instance, “weight loss” is common and often the sign of successful diet! (Well, at least temporarily successful, anyway. 😃) Obviously, if you know of a harmless reason why you have a red flag symptom, it isn’t really a red flag (duh!). But every single actual red flag — in combination with severe low back pain that’s been going on for several weeks — is definitely a good reason to get yourself checked out.

