Non-mechanical Disease Processes: Sometimes, non-mechanical disease processes like cancer, kidney stones, or a tumor may cause low back pain. These symptoms are usually, but not always, accompanied by other symptoms like unexpected weight loss, fever, or malaise that indicate a non-mechanical cause of your pain. These diseases are rare, but they can happen, so if your back pain continues for more than a few weeks after physical therapy treatment begins, a visit to your doctor is certainly in order to rule out a sinister problem.
As has been highlighted by research presented at the national meeting of the American College of Rheumatology, a very important aspect of the individual evaluation is the patient's own understanding and perception of their particular situation. British researchers found that those who believed that their symptoms had serious consequences on their lives and that they had, or treatments had, little control over their symptoms were more likely to have a poor outcome. This research points out to physicians the importance of addressing the concerns and perceptions that patients have about their condition during the initial evaluations.

Arthritis: The spondyloarthropathies are inflammatory types of arthritis that can affect the lower back and sacroiliac joints. Examples of spondyloarthropathies include reactive arthritis (Reiter's disease), ankylosing spondylitis, psoriatic arthritis, and the arthritis of inflammatory bowel disease. Each of these diseases can lead to low back pain and stiffness, which is typically worse in the morning. These conditions usually begin in the second and third decades of life. They are treated with medications directed toward decreasing the inflammation. Newer biologic medications have been greatly successful in both quieting the disease and stopping its progression. 
I’m not endorsing or saying these stretches are a miracle cure, but I definitely think they’ve helped. I’ve even started to add a few gentle yoga poses and pilates moves which I could so easily do, back in the day, when I was 63 kilos and participated in the greatest oxymoron ever named … a thing called the Fun Run. If I’m not careful, and I keep stretching away each day, I could end up with a 6 pack and back to my 5′ 7″ instead of 5′ 5″.

Irritable hip: What you need to know Irritable hip is a common cause of hip pain and limping in children before they reach puberty. It may happen after an injury or a viral infection, or because of poor blood flow. It usually gets better with rest within 2 weeks. Pain killers may help relieve symptoms. Those under 16 years should not use aspirin. Read now
Disc degeneration remains a key cause of chronic low back pain and the pain often persists despite surgery. NIH-funded basic science and preclinical studies are investigating molecular-level mechanisms that cause discs in the spine to degenerate, as well as protective mechanisms involved in disc remodeling that may diminish with advancing age. Such studies may help identify future therapeutic strategies to block degenerative mechanisms or promote remodeling processes. NIH also is funding early research on stem cell approaches to promote disc regeneration and rejuvenate cells of the nucleus pulposus, the jelly-like substance in the center of intervertebral discs that loses water content as people age.
Beacon Orthopaedics & Sports Medicine, Ltd. complies with applicable Federal civil rights laws and does not discriminate on the basis of race, color, national origin, age, disability, or sex. If you speak a language other than English, language assistance services, free of charge, are available to you. Call the Call Center at (513) 354-3700. Español (Spanish): ATENCIÓN: Si habla español, tiene a su disposición servicios gratuitos de asistencia lingüística. Llame al Call Center at (513) 354-3700. 繁體中文 (Chinese): 注意:如果您使用繁體中文,您可以免費獲得語言援助服務。請致電 Call Center at (513) 354-3700.
Since the hip flexors are so easy to overuse and strain, it is important to stretch them before exercise or strenuous activity. Because of their connectedness to other muscle groups in the legs (like the quadriceps), it is important to stretch the muscle group as a whole, not individually. This ensures that the entire area is warmed up and ready for the strain of exercise or activity, not just one or two individual muscles.
For example, your quadriceps muscles are a group of four that are located at the front of the thigh; one of the group members, the rectus femoris flexes the hip, which brings your lower extremity (thigh, lower leg, and foot) forward, in front of you. On the other hand, your hamstring muscles are located at the back of the thigh. When they contract, they extend the lower extremity, bringing it behind you.
Health Tools Baby Due Date CalculatorBasal Metabolic Rate CalculatorBody Mass Index (BMI) CalculatorCalories Burned CalculatorChild Energy Requirements CalculatorDaily Calcium Requirements CalculatorDaily Fibre Requirements CalculatorIdeal Weight CalculatorInfectious Diseases Exclusion Periods ToolOvulation CalculatorSmoking Cost CalculatorTarget Heart Rate CalculatorWaist-to-hip Ratio Calculator Risk Tests Depression Self-AssessmentErectile Dysfunction ToolMacular Degeneration ToolOsteoporosis Risk TestProstate Symptoms Self-Assessment
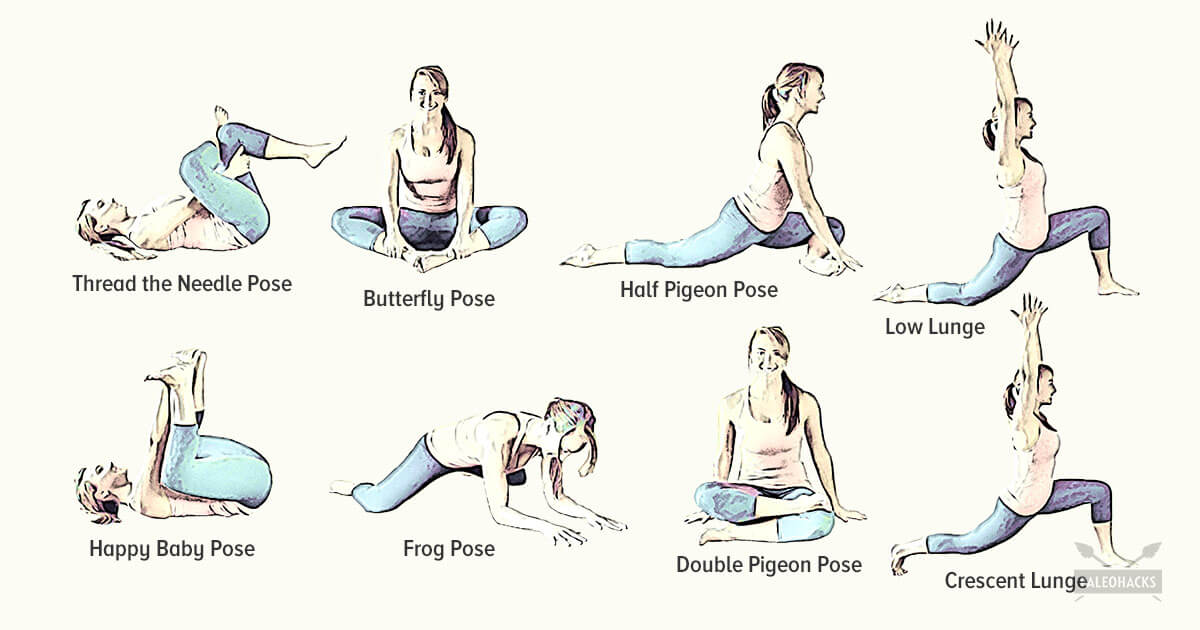

Start in a runner’s lunge with right leg forward, right knee over right ankle and back leg straight. Walk right foot over toward left hand, then drop right shin and thigh to the floor, making sure to keep right knee in line with right hip. Allow left leg to rest on the floor with top of left foot facing down. Take a moment to square your hips to the front of the room. Hold here, or hinge at hips and lower torso toward floor, allowing head to rest on forearms. Hold for at least 30 seconds, then repeat on opposite side. You want to feel a moderate stretch in the outside of the right thigh, but if this pose hurts your knees or feels too uncomfortable, stick with Thread the Needle. 
To stretch your quadriceps at the hip, the idea is to do the opposite movement to flexion, i.e., extension. You can perform extension moves at the hip while standing, lying on your side, lying prone (on your stomach) and kneeling. Even basic stretches done at a pain-free level where you can feel a small bit of challenge, and that are held continuously for approximately 30 seconds may translate to better posture and less back pain.
If you have hip pain, you may benefit from the skilled services of a physical therapist to help determine the cause of your pain. Your PT can work with you to develop a treatment strategy to treat your hip pain or hip discomfort. Understanding why your hip is hurting can help your physical therapist and doctor prescribe the right treatment regimen for your specific condition.

Tight hip flexors can also make it harder for your glutes to activate—since they're opposing muscle groups, when one is really tight the other becomes lengthened. When a muscle is more lengthened than it should be, it takes away some of its ability to contract. When your glutes are in this compromised position, it can cause other muscles to do more work than they should, making your workouts less efficient and sometimes, increasing your risk of injury.
How to do it: Grab a pair of dumbbells and stand with your feet slightly wider than hip-width apart, knees slightly bent. Hold the weights in front of your thighs, palms facing in. Maintaining a neutral spine, hinge forward from your hips, reaching the dumbbells to the ground, until your torso is almost parallel with the floor. Focus on using your glutes to raise your body halfway back up [as shown] and then return to full forward hinge again. That’s one rep. Repeat 20 times total.
Back pain can be confusing enough as it is. Sometimes it may be difficult deciphering if the pain is even coming from your back, and trying to figure out what causes it can be mind-boggling. And many experts recommend focusing on mechanical sources of your back pain rather than anatomical sources of your pain. Is it a herniated disc, bulging disc, or facet joint arthritis causing your problem? It can be hard to decide, so focusing on what you are doing and the positions you put your back in may be the best way to determine the cause of your back pain.


