Mechanical pain. By far the most common cause of lower back pain, mechanical pain (axial pain) is pain primarily from the muscles, ligaments, joints (facet joints, sacroiliac joints), or bones in and around the spine. This type of pain tends to be localized to the lower back, buttocks, and sometimes the top of the legs. It is usually influenced by loading the spine and may feel different based on motion (forward/backward/twisting), activity, standing, sitting, or resting.
Non-mechanical Disease Processes: Sometimes, non-mechanical disease processes like cancer, kidney stones, or a tumor may cause low back pain. These symptoms are usually, but not always, accompanied by other symptoms like unexpected weight loss, fever, or malaise that indicate a non-mechanical cause of your pain. These diseases are rare, but they can happen, so if your back pain continues for more than a few weeks after physical therapy treatment begins, a visit to your doctor is certainly in order to rule out a sinister problem.
You can use over-the-counter remedies such as Motrin or Advil (ibuprofen) or Aleve (naproxen) to help with pain and swelling. Tylenol (acetaminophen) works for pain relief, but it doesn't treat inflammation and swelling. If you have heart disease, high blood pressure, kidney disease, or if you've had ulcers or internal bleeding, check with your doctor before taking any of these medications.
Hip hikers (also known as the pelvic drop) are great exercises to get your gluteal muscles working in a weight bearing position. To do the exercise, stand sideways with one foot on a step and the other hanging off. Keeping both knees straight, lower down your pelvis on one side so your foot moves toward the floor. Both knees should remain straight; the motion should come from your hip joint. Once your pelvis is lowered down, slowly raise it back up to the starting position. Repeat the exercise for 10 repetitions.
Sit on floor with knees bent and shins stacked with right leg on top. Use your hand to position right ankle on left knee. Ideally, the right knee will rest on the left thigh, but if your hips are tight, your right knee may point up toward the ceiling (overtime, as your hips become more open, your knee will lower). Keeping your hips squared to the front of the room, hinge at the hips and slowly walk hands slightly forward. If this is enough of a stretch, hold here, or fold your torso over your thighs to go deeper. Hold for at least 30 seconds, then repeat on opposite side.
Try Atrogel: Atrogel is amazing when it comes to soothing and easing pain, helping to relieve muscle aches, stiffness and bruising. It’s prepared using extracts of fresh arnica flowers and can be applied up to 4 times a day! Suitable for pregnant women and children, simply apply this lovely non-greasy formula to the affected area for some much-needed relief!
The multifidus muscles run up and down along the back of the spine, and are important for keeping the spine straight and stable during many common movements such as sitting, walking and lifting.[12] A problem with these muscles is often found in someone with chronic low back pain, because the back pain causes the person to use the back muscles improperly in trying to avoid the pain.[31] The problem with the multifidus muscles continues even after the pain goes away, and is probably an important reason why the pain comes back.[31] Teaching people with chronic low back pain how to use these muscles is recommended as part of a recovery program.[31]
Electrodiagnostics are procedures that, in the setting of low back pain, are primarily used to confirm whether a person has lumbar radiculopathy. The procedures include electromyography (EMG), nerve conduction studies (NCS), and evoked potential (EP) studies. EMG assesses the electrical activity in a muscle and can detect if muscle weakness results from a problem with the nerves that control the muscles. Very fine needles are inserted in muscles to measure electrical activity transmitted from the brain or spinal cord to a particular area of the body. NCSs are often performed along with EMG to exclude conditions that can mimic radiculopathy. In NCSs, two sets of electrodes are placed on the skin over the muscles. The first set provides a mild shock to stimulate the nerve that runs to a particular muscle. The second set records the nerve’s electrical signals, and from this information nerve damage that slows conduction of the nerve signal can be detected. EP tests also involve two sets of electrodes—one set to stimulate a sensory nerve, and the other placed on the scalp to record the speed of nerve signal transmissions to the brain.
The condition is cauda equina syndrome. It involves “acute loss of function of the neurologic elements (nerve roots) of the spinal canal below the termination (conus) of the spinal cord,” where the nerves spread out like a horse (equina) tail. Again, this condition causes symptoms in the “saddle” of the body: butt, groin, inner thighs. BACK TO TEXT
Kneel on your mat with your thighs perpendicular to the floor and tops of your feet facing down. Bring your inner knees together. Slide your feet apart so they are slightly wider than your hips and press the tops of your feet evenly into the mat. Slowly sit down between your feet. Use your hands to turn the top of your thighs inward. Then, lean back onto your forearms and slowly lower torso to floor. Hold for at least 30 seconds.
Acupuncture is no better than placebo, usual care, or sham acupuncture for nonspecific acute pain or sub-chronic pain.[87] For those with chronic pain, it improves pain a little more than no treatment and about the same as medications, but it does not help with disability.[87] This pain benefit is only present right after treatment and not at follow-up.[87] Acupuncture may be a reasonable method to try for those with chronic pain that does not respond to other treatments like conservative care and medications.[1][88]

Pregnancy symptoms can vary from woman to woman, and not all women experience the same symptoms. When women do experience pregnancy symptoms they may include symptoms include missed menstrual period, mood changes, headaches, lower back pain, fatigue, nausea, breast tenderness, and heartburn. Signs and symptoms in late pregnancy include leg swelling and shortness of breath. Options for relief of pregnancy symptoms include exercise, diet, and other lifestyle changes.
For those with pain localized to the lower back due to disc degeneration, fair evidence supports spinal fusion as equal to intensive physical therapy and slightly better than low-intensity nonsurgical measures.[15] Fusion may be considered for those with low back pain from acquired displaced vertebra that does not improve with conservative treatment,[14] although only a few of those who have spinal fusion experience good results.[15] There are a number of different surgical procedures to achieve fusion, with no clear evidence of one being better than the others.[83] Adding spinal implant devices during fusion increases the risks but provides no added improvement in pain or function.[11]

Biofeedback is used to treat many acute pain problems, most notably back pain and headache. The therapy involves the attachment of electrodes to the skin and the use of an electromyography machine that allows people to become aware of and selfregulate their breathing, muscle tension, heart rate, and skin temperature. People regulate their response to pain by using relaxation techniques. Biofeedback is often used in combination with other treatment methods, generally without side effects. Evidence is lacking that biofeedback provides a clear benefit for low back pain.
Congenital bone conditions: Congenital causes (existing from birth) of low back pain include scoliosis and spina bifida. Scoliosis is a sideways (lateral) curvature of the spine that can be caused when one lower extremity is shorter than the other (functional scoliosis) or because of an abnormal architecture of the spine (structural scoliosis). Children who are significantly affected by structural scoliosis may require treatment with bracing and/or surgery to the spine. Adults infrequently are treated surgically but often benefit by support bracing. Spina bifida is a birth defect in the bony vertebral arch over the spinal canal, often with absence of the spinous process. This birth defect most commonly affects the lowest lumbar vertebra and the top of the sacrum. Occasionally, there are abnormal tufts of hair on the skin of the involved area. Spina bifida can be a minor bony abnormality without symptoms. However, the condition can also be accompanied by serious nervous abnormalities of the lower extremities.

In terms of diagnosing hip pain, typically a patient will expect when they come in to be asked about their symptoms, and it’s very important to find out when did these symptoms start, how long they have been going on, how frequent they are, if they come on in the morning or the evening, do they come on with any certain activity, and if there is something that makes it better or worse. The intensity of the pain is also important. Does it have any associated radiating symptoms? Is it localized in one spot or does it move? After getting a history and finding out what type of pain the patient is having, which also includes whether the pain is dull, aching, sharp, or intense, then it’s important to do a good physical exam. The physical examination involves testing the muscle strength, testing for sensation, doing provocative maneuvers which might help us rule out one type of injury from another.
Or anything else. Pain is a poor indicator, period! The human nervous system is really terrible about this: it routinely produces false alarms, and alarms that are much too loud. See Pain is Weird: Pain science reveals a volatile, misleading sensation that is often more than just a symptom, and sometimes worse than whatever started it. BACK TO TEXT

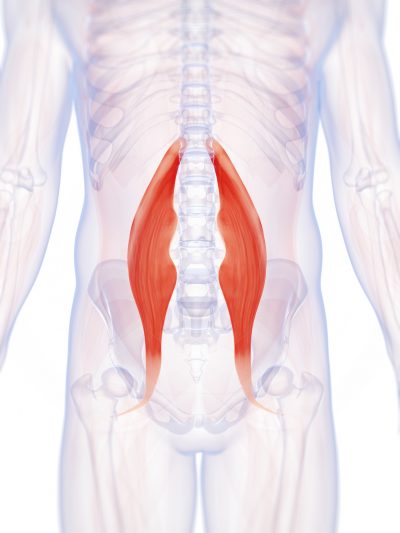
Tight hip flexors can result in lower back pain, hip pain and injury. A lot of strain is put on those muscles during activities that involve sprinting and kicking. For example, runners are more prone to hip flexor injuries because of the small, repetitive movement during running. But even if you’re not an athlete, hip flexor injuries can occur during everyday activities (for instance, slipping and falling or running to catch a bus). When those tight muscles are suddenly stretched beyond what they are accustomed to, you might also experience pain in the upper groin region, typically where the hip meets the pelvis.
Muscle Imbalances – The front of your hips, your hip flexors, are the muscles that will tighten and shorten while you are sitting for hours each day. While you are sitting, the back of your hips, your glutes and your hip extensors, are being overstretched. But just because they are being tightened and stretched respectively, doesn’t benefit either of them. They are also being weakened because of the lack of use of each muscle group.
"As compared to a conventional deadlift, the sumo allows for greater recruitment of the adductors and a more stabilizing emphasis for the abductors," says Lindsey Cormack, a competitive powerlifter and CrossFit trainer. "Training sumo may feel less stable at first, but the balance requirement is what allows you to effectively train both the abductors and adductors."
Medications: A wide range of medications are used to treat acute and chronic low back pain. Some are available over the counter (OTC); others require a physician’s prescription. Certain drugs, even those available OTC, may be unsafe during pregnancy, may interact with other medications, cause side effects, or lead to serious adverse effects such as liver damage or gastrointestinal ulcers and bleeding. Consultation with a health care provider is advised before use. The following are the main types of medications used for low back pain:
Osteoarthritis. This condition results from wear and tear of the disc and facet joints. It causes pain, inflammation, instability, and stenosis to a variable degree, and can occur at a single level or multiple levels of the lower spine. Spinal osteoarthritis is associated with aging and is slowly progressive. It is also referred to as spondylosis or degenerative joint disease.
^ Enke, Oliver; New, Heather A.; New, Charles H.; Mathieson, Stephanie; McLachlan, Andrew J.; Latimer, Jane; Maher, Christopher G.; Lin, C.-W. Christine (2 July 2018). "Anticonvulsants in the treatment of low back pain and lumbar radicular pain: a systematic review and meta-analysis". Canadian Medical Association Journal. 190 (26): E786–E793. doi:10.1503/cmaj.171333. PMC 6028270. PMID 29970367.
3. Tendinitis and bursitis Many tendons around the hip connect the muscles to the joint. These tendons can easily become inflamed if you overuse them or participate in strenuous activities. One of the most common causes of tendinitis at the hip joint, especially in runners, is iliotibial band syndrome — the iliotibial band is the thick span of tissue that runs from the outer rim of your pelvis to the outside of your knee.
The lumbar (or lower back) region is made up of five vertebrae (L1–L5), sometimes including the sacrum. In between these vertebrae are fibrocartilaginous discs, which act as cushions, preventing the vertebrae from rubbing together while at the same time protecting the spinal cord. Nerves come from and go to the spinal cord through specific openings between the vertebrae, providing the skin with sensations and messages to muscles. Stability of the spine is provided by the ligaments and muscles of the back and abdomen. Small joints called facet joints limit and direct the motion of the spine.[30]
Strength training is another key part of the “do” category, Dr. Vasileff says. “It’s a good idea to focus on quad, hamstring, and glute strength,” he says. These muscles surround your hips and provide support, along with your core—which is another area to focus on. “Strengthening your core helps to normalize your walking pattern and stabilize how your pelvis and hips move,” Dr. Vasileff says. That translates to less pain and better hip mobility.
I had compromised range of motion in my hips. I am a runner and I couldn’t increase my speed. Using this program – http://certifiedtreatment.com/hipflexors I adjusted my back and relieved the pain the tightness in my hips and lower back which allowed me to run harder and longer. Not only do I have less pain on a daily basis, but I also have more energy and stamina when I run. I find myself with better movement and sleep, and I have maximized my performance.
NINDS-funded studies are contributing to a better understanding of why some people with acute low back pain recover fully while others go on to develop chronic low back pain. Brain imaging studies suggest that people with chronic low back pain have changes in brain structure and function. In one study, people with subacute back pain were followed for one year. Researchers found that certain patterns of functional connectivity across brain networks correlated with the likelihood of pain becoming chronic. The findings suggest that such patterns may help predict who is most likely to transition from subacute to chronic back pain. Other research seeks to determine the role of brain circuits important for emotional and motivational learning and memory in this transition, in order to identify new preventive interventions.