Contour Sleep Knee Spacer: Correct sleep alignment is a critical component to rehabilitating an injured hip. This device can help to decrease pressure to the legs and hips while you sleep. Perfect for side sleepers, the Contour Sleep Knee Spacer fits softly between the knees without disrupting your sleep. It helps tense muscles relax and lets you have a better night’s sleep free from painful hip tension.
I’m not endorsing or saying these stretches are a miracle cure, but I definitely think they’ve helped. I’ve even started to add a few gentle yoga poses and pilates moves which I could so easily do, back in the day, when I was 63 kilos and participated in the greatest oxymoron ever named … a thing called the Fun Run. If I’m not careful, and I keep stretching away each day, I could end up with a 6 pack and back to my 5′ 7″ instead of 5′ 5″.

Spondylolisthesis. This condition occurs when one vertebra slips over the adjacent one. There are 5 types of spondylolisthesis but the most common are secondary to a defect or fracture of the pars (between the facet joints) or mechanical instability of the facet joints (degenerative). The pain can be caused by instability (back) or compression of the nerves (leg).
Deanna is an ACE® certified personal trainer, Balanced Body® Pilates instructor, and NASM® Fitness Nutrition Specialist. She is passionate about inspiring others to lead a healthier lifestyle through fun workouts and healthy food. When she’s not creating new workouts and recipes for her blog The Live Fit Girls she enjoys running with her two dogs and traveling.
Parts of the pain sensation and processing system may not function properly; creating the feeling of pain when no outside cause exists, signaling too much pain from a particular cause, or signaling pain from a normally non-painful event. Additionally, the pain modulation mechanisms may not function properly. These phenomena are involved in chronic pain.[12]

Lumbar strain (acute, chronic): A lumbar strain is a stretch injury to the ligaments, tendons, and/or muscles of the low back. The stretching incident results in microscopic tears of varying degrees in these tissues. Lumbar strain is considered one of the most common causes of low back pain. The injury can occur because of overuse, improper use, or trauma. Soft-tissue injury is commonly classified as "acute" if it has been present for days to weeks. If the strain lasts longer than three months, it is referred to as "chronic." Lumbar strain most often occurs in people in their 40s, but it can happen at any age. The condition is characterized by localized discomfort in the low back area with onset after an event that mechanically stressed the lumbar tissues. The severity of the injury ranges from mild to severe, depending on the degree of strain and resulting spasm of the muscles of the low back. The diagnosis of lumbar strain is based on the history of injury, the location of the pain, and exclusion of nervous system injury. Usually, X-ray testing is only helpful to exclude bone abnormalities.
Physician specialties that evaluate and treat low back pain range from generalists to subspecialists.These specialties include emergency medicine physicians, general medicine, family medicine, internal medicine, gynecology, spine surgeons (orthopaedics and neurosurgery), rheumatology, pain management, and physiatry. Other health care providers for low back pain include physical therapists, chiropractors, massage therapists, psychologists, and acupuncturists.

Paget's disease can be diagnosed on plain X-rays. However, a bone biopsy is occasionally necessary to ensure the accuracy of the diagnosis. Bone scanning is helpful to determine the extent of the disease, which can involve more than one bone area. A blood test, alkaline phosphatase, is useful for diagnosis andmonitoring response to therapy. Treatment options include aspirin, other anti-inflammatory medicines, pain medications, and medications that slow therate of bone turnover, such as calcitonin (Calcimar, Miacalcin), etidronate (Didronel), alendronate (Fosamax), risedronate (Actonel), and pamidronate (Aredia).
Epidural injections of steroid drugs are frequently used to treat sciatica, despite limited evidence for their effectiveness. Moreover, these treatments are based on the assumption that reducing local inflammation in the vertebral column will relieve pain, but an association between structural abnormalities, inflammation, and sciatica symptoms has not been clearly demonstrated. NINDS-funded researchers are using a new imaging technique that can detect inflammation to better understand what causes chronic sciatica pain and to provide evidence to inform treatment selection.
Strengthening exercises, beyond general daily activities, are not advised for acute low back pain, but may be an effective way to speed recovery from chronic or subacute low back pain. Maintaining and building muscle strength is particularly important for persons with skeletal irregularities. Health care providers can provide a list of beneficial exercises that will help improve coordination and develop proper posture and muscle balance. Evidence supports short- and long-term benefits of yoga to ease chronic low back pain.
If certain activities or overuse are causing hip pain, stop those that aggravate the discomfort and talk to your doctor. Excess weight can put pressure on the hip joint, so losing the pounds can provide relief and help you avoid further problems. Some causes of hip pain, such as fractures or hernias, may need surgical repairs. If your hip pain persists, talk to your doctor about the possible causes and treatments.
These exercises can be done three to five times per week; be sure to build in a rest day here or there to allow your hip muscles to recover. Working to strengthen your knees and ankles can be done as well to be sure you completely work all muscles groups of your lower extremities. Remember, your ankle and knee muscles help control the position of your hips, just as your hip muscles control the position of your knees and ankles. They all work together in a kinetic chain.

Simply stand up straight with your feet about shoulder-width apart. Slowly bend your knees and hips, lowering yourself until your knees obscure your toes or you achieve a 90 degree angle. Hold for a count of 5 and then gently resume your original position. This can be a tough one so again, don’t overdo it and hold on to a table if you need a little extra support! Try to repeat between 5-10 times.
Arthritis: The spondyloarthropathies are inflammatory types of arthritis that can affect the lower back and sacroiliac joints. Examples of spondyloarthropathies include reactive arthritis (Reiter's disease), ankylosing spondylitis, psoriatic arthritis, and the arthritis of inflammatory bowel disease. Each of these diseases can lead to low back pain and stiffness, which is typically worse in the morning. These conditions usually begin in the second and third decades of life. They are treated with medications directed toward decreasing the inflammation. Newer biologic medications have been greatly successful in both quieting the disease and stopping its progression.

The hip joint is designed to withstand a fair amount of wear and tear, but it’s not indestructible. For example, when you walk, a cushion of cartilage helps prevent friction as the hip bone moves in its socket. With age and use, this cartilage can wear down or become damaged, or the hip bone itself can be fractured during a fall. In fact, more than 300,000 adults over 65 are hospitalized for hip fractures each year, according to the Agency for Healthcare Research and Quality.

Really a great content. Let me tell you first about hip flexor it is the engine through which our body moves. They control balance, our ability to sit, stand, twist, reach, bend, walk and step. One of my patient also suffering from same problem but due to lack of money he was unable to afford a treatment. So i recommend him a program to unlock hip flexor. If anyone wants they can check it out here ;- https://tinyurl.com/y8yaqs2s Report
Tight hip flexors can also make it harder for your glutes to activate—since they're opposing muscle groups, when one is really tight the other becomes lengthened. When a muscle is more lengthened than it should be, it takes away some of its ability to contract. When your glutes are in this compromised position, it can cause other muscles to do more work than they should, making your workouts less efficient and sometimes, increasing your risk of injury.

In this study, one patient with sciatica was sent for ten MRIs, which produced 49 distinct “findings,” 16 of them unique, none of which occurred in all ten reports. On average, each radiologist made about a dozen errors, seeing one or two things that weren’t there and missing about ten things that were. Yikes. Read a more detailed and informal description of this study.

Stretching is your next move, but not just any stretches. “Before your workout, you want to go for dynamic stretches, or stretches that put the joint through a full range of motion,” says Lefkowith. Moves like squats and lunges will get your muscles fired up (especially if you focus on squeezing your butt at the top of those squats), says Lefkowith.
Injury to the bones and joints: Fractures (breakage of bone) of the lumbar spine and sacrum bone most commonly affect elderly people with osteoporosis, especially those who have taken long-term cortisone medication. For these individuals, occasionally even minimal stresses on the spine (such as bending to tie shoes) can lead to bone fracture. In this setting, the vertebra can collapse (vertebral compression fracture). The fracture causes an immediate onset of severe localized pain that can radiate around the waist in a band-like fashion and is made intensely worse with body motions. This pain generally does not radiate down the lower extremities. Vertebral fractures in younger patients occur only after severe trauma, such as from motor-vehicle accidents or a convulsive seizure.
Long periods of inactivity in bed are no longer recommended, as this treatment may actually slow recovery. Spinal manipulation for periods of up to one month has been found to be helpful in some patients who do not have signs of nerve irritation. Future injury is avoided by using back-protection techniques during activities and support devices as needed at home or work.

If low back pain gets worse or does not improve after two to three days of home treatment, contact a primary-care physician. The physician can evaluate the patient and perform a neurological exam in the office to determine which nerve root is being irritated, as well as rule out other serious medical conditions. If there are clear signs that the nerve root is being compressed, a physician can prescribe medications to relieve the pain, swelling and irritation; he or she also may recommend limitation of activities. If these treatment options do not provide relief within two weeks, it may be time to consider other diagnostic studies and possibly surgery.
MRI and x-ray for low back pain are surprisingly unreliable,1 because things like bulging discs usually aren’t a deal,2 most back pain goes away on its own,3 and trigger points (“muscle knots”) are common and can be alarmingly intense but aren’t dangerous.4 Most patients are much better off when they feel confident about these things. The power of justified, rational confidence is a huge factor in back pain.5 Sadly, many healthcare professionals continue to perpetuate the idea of fragile backs,6 which undermines that valuable confidence.

If your hips are killing you, you probably spend a lot of time sitting – in the car, at work, on that spinning seat – which puts your hips in near-constant “flexion”, says Cori Lefkowith, NASM-certified personal trainer and owner of Redefining Strength in Orange County, California. Even running involves a repetitive flexion movement that can cause pain.

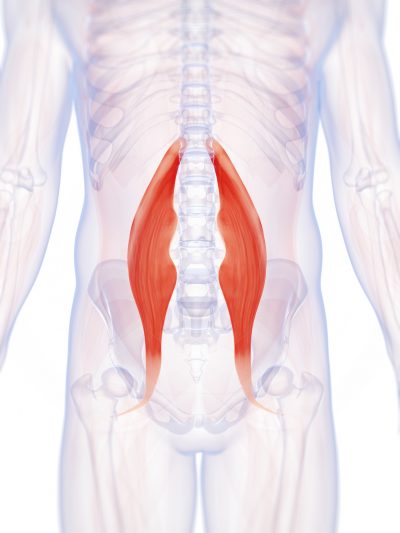
The main work of your hip flexors is to bring your knee toward your chest and to bend at the waist. Symptoms associated with a hip flexor strain can range from mild to severe and can impact your mobility. If you don’t rest and seek treatment, your hip flexor strain symptoms could get worse. But there are many at-home activities and remedies that can help reduce hip flexor strain symptoms.
Bone scans are used to detect and monitor infection, fracture, or disorders in the bone. A small amount of radioactive material is injected into the bloodstream and will collect in the bones, particularly in areas with some abnormality. Scanner-generated images can be used to identify specific areas of irregular bone metabolism or abnormal blood flow, as well as to measure levels of joint disease.

The hip is a very stable ball and socket type joint with an inherently large range of motion. The hip contains some of the largest muscle in the body as well as some of the smallest. Most people lack mobility due to a relatively sedentary lifestyle. Periods of prolonged sitting results in tightness of the hip flexors and hamstrings. Tightness in the muscles and ligaments can created joint forces that result in arthritis, postural problems, bursitis, and mechanical back pain.
Results after four years of follow-up showed that in general, otherwise healthy people who have surgery for one of these three conditions are likely to fare better than those who receive non-operative care. However, the results also indicated that people who are reluctant to have surgery may also recover with non-operative treatments if their conditions are not progressing and their pain is tolerable, and importantly, delaying or avoiding surgery did not cause additional damage in most cases. Researchers are continuing to track SPORT patient cohorts over a nine-year follow-up period to assess longer term treatment results and cost effectiveness across treatment options. In the interest of improving surgical techniques, NIH also is funding research on factors that contribute to the success or failure of artificial disc replacement surgery, including studies to compare discs on the market for significant differences in their durability rates over time.
The treatment of lumbar strain consists of resting the back (to avoid reinjury), medications to relieve pain and muscle spasm, local heat applications, massage, and eventual (after the acute episode resolves) reconditioning exercises to strengthen the low back and abdominal muscles. Initial treatment at home might include heat application, acetaminophen (Tylenol) or ibuprofen (Advil, Motrin), and avoiding reinjury and heavy lifting. Prescription medications that are sometimes used for acute low back pain include anti-inflammatory medications, such as sulindac (Clinoril), naproxen (Naprosyn), and ketorolac (Toradol) by injection or by mouth, muscle relaxants, such as carisoprodol (Soma), cyclobenzaprine (Flexeril), methocarbamol (Robaxin), and metaxalone (Skelaxin), as well as analgesics, such as tramadol (Ultram).

Or anything else. Pain is a poor indicator, period! The human nervous system is really terrible about this: it routinely produces false alarms, and alarms that are much too loud. See Pain is Weird: Pain science reveals a volatile, misleading sensation that is often more than just a symptom, and sometimes worse than whatever started it. BACK TO TEXT
Most functional exercises—ones that mimic everyday movements such as squats, hip hinges (deadlifts, for example), lunges, steps-ups—stretch and strengthen your hip muscles in some way. So if you strength train and do a variety of these sorts of movements, you're probably working these important muscles without even realizing it. On the other hand, if you mostly focus on exercise methods that have you doing the same movement over and over again, like running or cycling, there's a good chance your hips aren't as strong as they should be. And that can have a negative impact on not only your workouts, but how you move through life in general.
The big idea of classification-based cognitive functional therapy (CB-CFT or just CFT) is that most back pain has nothing to do with scary spinal problems and so the cycle of pain and disability can be broken by easing patient fears and anxieties. For this study, CFT was tried with 62 patients and compared to 59 who were treated with manual therapy and exercise. The CFT group did better: a 13-point boost on a 100-point disability scale, and 3 points on a 10-point pain scale. As the authors put it for BodyInMind.org, “Disabling back pain can change for the better with a different narrative and coping strategies.” These results aren’t proof that the confidence cure works, but they are promising.
Radicular pain. This type of pain can occur if a spinal nerve root becomes impinged or inflamed. Radicular pain may follow a nerve root pattern or dermatome down into the buttock and/or leg. Its specific sensation is sharp, electric, burning-type pain and can be associated with numbness or weakness (sciatica). It is typically felt on only one side of the body.

Medicine FinderLatest NewsSlip, slap, slop early to save your skinComplementary medicine users have worse cancer survivalVideo: BoredomPut down the tablet; pick up a bookVideo: Lift your mood with some weightsQuicken your step to live longerThis web site is intended for Australian residents and is not a substitute for independent professional advice. Information and interactions contained in this Web site are for information purposes only and are not intended to be used to diagnose, treat, cure or prevent any disease. Further, the accuracy, currency and completeness of the information available on this Web site cannot be guaranteed. Tonic Digital Media Pty Ltd, its affiliates and their respective servants and agents do not accept any liability for any injury, loss or damage incurred by use of or reliance on the information made available via or through myDr whether arising from negligence or otherwise. See Privacy Policy and Disclaimer.2001-2019 myDr.com.au © | All Rights Reserved About UsContact UsDisclaimerPrivacy PolicyAdvertising PolicySitemap

If you’re worried you’re headed toward a surgeon’s office, there might be hope. According to the Arthritis Foundation, the best way to avoid hip replacement surgery is to get active in an exercise program. In a study, people who participated in an exercise program for 12 weeks were 44 percent less likely to need joint-replacement surgery six years later than those who did not exercise.
Toggle navigationNewsConditionsConditionsADHDAllergic rhinitisAlzheimer's diseaseAnxietyArthritisAsthmaAutismBowel cancerBreast cancerCancerChesty coughsChickenpoxChlamydiaCholesterolCoeliac diseaseCommon coldConstipationCOPDDepressionDiabetesDiverticulitisEpilepsyFatty liverFibromyalgiaGenital herpesGORD (reflux)GoutHaemorrhoidsHair lossHeart attackHepatitisHiatus herniaHigh blood pressureHIV and AIDSImpotenceMenopauseMigraineNeuropathic painOsteoporosisPainPeptic ulcersPneumoniaProstate cancerScabiesSchizophreniaSciaticaShinglesSinusitisSkin cancerStrokeThyroid gland disordersUrticaria (hives)Vaginal thrushVasectomyVertigoVulval problemsWhooping coughMedicinesMedicinesAugmentinAvilChlorsigDaklinzaDuromineEndepEndoneHarvoniLevlenLyricaMersyndolMetrogylPanadeine FortePanefcortelonePrimolutRestavitSovaldiStemetilViagraZentelFind a MedicineMedicines CentreSymptomsSymptomsBack painChildhood rashesCommon coldDepressionFeverFibromyalgiaHeart attackHeel painHerpesLeg acheLeg crampsSciaticaShinglesStrokeVaginal thrushVertigoMore symptomsLifestyleHealthy LifestyleAddictionsAlcoholCholesterolExerciseHealthy eatingHealthy WeightHeart healthImmunisationSleepSmokingStress Health Centres Nutrition & WeightSports & FitnessTools Medical Dictionary Medical Dictionary
Your hip labrum is a band of cartilage-like tissue that courses around the outer rim of your hip socket. This labrum helps to support the joint and deepen the socket. Sometimes overuse or an injury to your hip can cause a tear in your labrum. A hip labrum tear may result in a condition called femoroacetabular impingement (FAI). When this happens, hip pain may result, and exercises to stretch and stabilize your hip may be performed.
Tight hip flexors can result in lower back pain, hip pain and injury. A lot of strain is put on those muscles during activities that involve sprinting and kicking. For example, runners are more prone to hip flexor injuries because of the small, repetitive movement during running. But even if you’re not an athlete, hip flexor injuries can occur during everyday activities (for instance, slipping and falling or running to catch a bus). When those tight muscles are suddenly stretched beyond what they are accustomed to, you might also experience pain in the upper groin region, typically where the hip meets the pelvis.
Imaging is indicated when there are red flags, ongoing neurological symptoms that do not resolve, or ongoing or worsening pain.[5] In particular, early use of imaging (either MRI or CT) is recommended for suspected cancer, infection, or cauda equina syndrome.[5] MRI is slightly better than CT for identifying disc disease; the two technologies are equally useful for diagnosing spinal stenosis.[5] Only a few physical diagnostic tests are helpful.[5] The straight leg raise test is almost always positive in those with disc herniation.[5] Lumbar provocative discography may be useful to identify a specific disc causing pain in those with chronic high levels of low back pain.[41] Similarly, therapeutic procedures such as nerve blocks can be used to determine a specific source of pain.[5] Some evidence supports the use of facet joint injections, transforminal epidural injections and sacroilliac injections as diagnostic tests.[5] Most other physical tests, such as evaluating for scoliosis, muscle weakness or wasting, and impaired reflexes, are of little use.[5]

The medication typically recommended first are NSAIDs (though not aspirin) or skeletal muscle relaxants and these are enough for most people.[13][6] Benefits with NSAIDs; however, is often small.[67] High-quality reviews have found acetaminophen (paracetamol) to be no more effective than placebo at improving pain, quality of life, or function.[68][69] NSAIDs are more effective for acute episodes than acetaminophen; however, they carry a greater risk of side effects including: kidney failure, stomach ulcers and possibly heart problems. Thus, NSAIDs are a second choice to acetaminophen, recommended only when the pain is not handled by the latter. NSAIDs are available in several different classes; there is no evidence to support the use of COX-2 inhibitors over any other class of NSAIDs with respect to benefits.[70][13][71] With respect to safety naproxen may be best.[72] Muscle relaxants may be beneficial.[13]
Low back pain can be caused by tumors, either benign or malignant, that originate in the bone of the spine or pelvis and spinal cord (primary tumors) and those which originate elsewhere and spread to these areas (metastatic tumors). Symptoms range from localized pain to radiating severe pain and loss of nerve and muscle function (even incontinence of urine and stool) depending on whether or not the tumors affect the nervous tissue. Tumors of these areas are detected using imaging tests, such as plain X-rays, nuclear bone scanning, and CAT and MRI scanning.

Kneel with a wall or pillar behind you, knees hips-width apart and toes touching the wall. Arch your back to lean back while keeping your hips stacked over your knees. Take your arms overhead and touch your palms into the wall behind you. This bend does not need to be extremely deep to feel a great stretch in the hips and strength in the lower back.

Along with these exercises, it's also important to do some supplementary exercises to work your hip's supporting muscles. You've probably heard of your shoulder's rotator cuff. Well, your hip also has a cuff, or a group of muscles that help stabilize and support movement. For these exercises, you'll need a mini-band, a longer thera-band or tubing (both are sold at many sporting goods stores, or can be purchased online), and a cable-column unit.
Im a skateboarder and a couple weeks ago i skated alot every day and my lefy hip was starting to get sore. But of course i couldnt resist skating so i kept skating and it got worse and worse to the point i couldnt really skate at all without my hip hurting but of course i would still mess around on the board doing tiny tricks but a couple days ago i was just skating around not really doing tricks and i slipped and kicked my leg out and REALLY hurt my hip and thought i tore a tendon or something and couldnt walk for two days, but its gotten alot better and i can walk fairly normal and i ice it everyday but whenever i stretch it its just a really sharp pain it doesnt feel like im stretching it. What do i do when all the stretch does is make a sharp pain? How do i strengthen my hip? And how long would it take to strengthen my hip to full strength again? Because i cant stand not being able to skate. Please reply so i can skate as soon as possible thank you

Low back pain can be caused by tumors, either benign or malignant, that originate in the bone of the spine or pelvis and spinal cord (primary tumors) and those which originate elsewhere and spread to these areas (metastatic tumors). Symptoms range from localized pain to radiating severe pain and loss of nerve and muscle function (even incontinence of urine and stool) depending on whether or not the tumors affect the nervous tissue. Tumors of these areas are detected using imaging tests, such as plain X-rays, nuclear bone scanning, and CAT and MRI scanning.
Imaging is indicated when there are red flags, ongoing neurological symptoms that do not resolve, or ongoing or worsening pain.[5] In particular, early use of imaging (either MRI or CT) is recommended for suspected cancer, infection, or cauda equina syndrome.[5] MRI is slightly better than CT for identifying disc disease; the two technologies are equally useful for diagnosing spinal stenosis.[5] Only a few physical diagnostic tests are helpful.[5] The straight leg raise test is almost always positive in those with disc herniation.[5] Lumbar provocative discography may be useful to identify a specific disc causing pain in those with chronic high levels of low back pain.[41] Similarly, therapeutic procedures such as nerve blocks can be used to determine a specific source of pain.[5] Some evidence supports the use of facet joint injections, transforminal epidural injections and sacroilliac injections as diagnostic tests.[5] Most other physical tests, such as evaluating for scoliosis, muscle weakness or wasting, and impaired reflexes, are of little use.[5]
Most low back pain is acute, or short term, and lasts a few days to a few weeks. It tends to resolve on its own with self-care and there is no residual loss of function. The majority of acute low back pain is mechanical in nature, meaning that there is a disruption in the way the components of the back (the spine, muscle, intervertebral discs, and nerves) fit together and move.
Electrodiagnostics are procedures that, in the setting of low back pain, are primarily used to confirm whether a person has lumbar radiculopathy. The procedures include electromyography (EMG), nerve conduction studies (NCS), and evoked potential (EP) studies. EMG assesses the electrical activity in a muscle and can detect if muscle weakness results from a problem with the nerves that control the muscles. Very fine needles are inserted in muscles to measure electrical activity transmitted from the brain or spinal cord to a particular area of the body. NCSs are often performed along with EMG to exclude conditions that can mimic radiculopathy. In NCSs, two sets of electrodes are placed on the skin over the muscles. The first set provides a mild shock to stimulate the nerve that runs to a particular muscle. The second set records the nerve’s electrical signals, and from this information nerve damage that slows conduction of the nerve signal can be detected. EP tests also involve two sets of electrodes—one set to stimulate a sensory nerve, and the other placed on the scalp to record the speed of nerve signal transmissions to the brain.
Tight hip flexors can also make it harder for your glutes to activate—since they're opposing muscle groups, when one is really tight the other becomes lengthened. When a muscle is more lengthened than it should be, it takes away some of its ability to contract. When your glutes are in this compromised position, it can cause other muscles to do more work than they should, making your workouts less efficient and sometimes, increasing your risk of injury.
Nerve block therapies aim to relieve chronic pain by blocking nerve conduction from specific areas of the body. Nerve block approaches range from injections of local anesthetics, botulinum toxin, or steroids into affected soft tissues or joints to more complex nerve root blocks and spinal cord stimulation. When extreme pain is involved, low doses of drugs may be administered by catheter directly into the spinal cord. The success of a nerve block approach depends on the ability of a practitioner to locate and inject precisely the correct nerve. Chronic use of steroid injections may lead to increased functional impairment.

Those are some great stretches! I own a personal training studio in Severna Park, Maryland. Majority of my clients have physical limitations – so it’s important for them to stay flexible. I send these to my clients and even do these exercises for myself. I highly recommend these stretches to anyone, even people without physical limitations. I love the fact these are actually videos and not just stretches because it’s so much easier for people to figure out how to perform the stretches. You guys are the real MVP!
Deanna is an ACE® certified personal trainer, Balanced Body® Pilates instructor, and NASM® Fitness Nutrition Specialist. She is passionate about inspiring others to lead a healthier lifestyle through fun workouts and healthy food. When she’s not creating new workouts and recipes for her blog The Live Fit Girls she enjoys running with her two dogs and traveling.

In this study, one patient with sciatica was sent for ten MRIs, which produced 49 distinct “findings,” 16 of them unique, none of which occurred in all ten reports. On average, each radiologist made about a dozen errors, seeing one or two things that weren’t there and missing about ten things that were. Yikes. Read a more detailed and informal description of this study.

If you develop a sudden onset of low back pain, a visit to your physical therapist can help you determine the correct things to do to manage your acute pain. Your physical therapist should be able to analyze your lifestyle, movements, and overall medical history to help determine the likely cause of your pain. By focusing on these mechanical causes of back pain, you can make a change that may give you relief.
Sit on floor with knees bent and shins stacked with right leg on top. Use your hand to position right ankle on left knee. Ideally, the right knee will rest on the left thigh, but if your hips are tight, your right knee may point up toward the ceiling (overtime, as your hips become more open, your knee will lower). Keeping your hips squared to the front of the room, hinge at the hips and slowly walk hands slightly forward. If this is enough of a stretch, hold here, or fold your torso over your thighs to go deeper. Hold for at least 30 seconds, then repeat on opposite side.


