Pain in the hip can result from a number of factors. Sometimes diseases that affect other joints in the body, such as the inflammation resulting from arthritis, can be the cause of pain in the hip. Depending upon the cause of hip pain, the pain may occur when walking, running, or engaging in activity. Trochanteric bursitis is the most common type of hip bursitis and causes pain at the point of the hip.
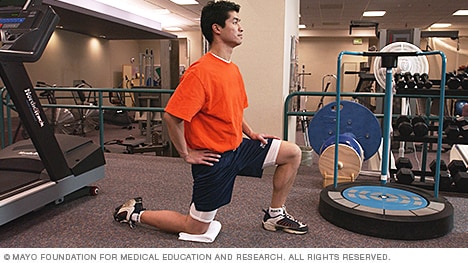
A sedentary lifestyle can lead to having weak and tight hip flexors as they are always in the shortened position. Tight hip flexors can lead to a limited range of motion, poor posture, lower back, and hip pain, and even injuries. These muscles need to get a workout when you are standing and doing movements such as raising your leg to climb stairs, run, or ride a bicycle.
Low back pain that lasts at least one day and limits activity is a common complaint.[7] Globally, about 40% of people have LBP at some point in their lives,[7] with estimates as high as 80% of people in the developed world.[22] Approximately 9 to 12% of people (632 million) have LBP at any given point in time, and nearly one quarter (23.2%) report having it at some point over any one-month period.[7][8] Difficulty most often begins between 20 and 40 years of age.[1] Low back pain is more common among people aged 40–80 years, with the overall number of individuals affected expected to increase as the population ages.[7]
Place a mini band around your ankles and spread your feet about shoulder-width apart. Keeping your legs relatively straight (you want the motion to come from your hips) and toes pointing forward, walk forward 10 steps, then backward 10 steps. Take a short break and then walk to the right 10 steps, then to the left 10 steps. Again, focus on keeping your legs straight and toes pointing forward. 
In diagnosing the causes of hip pain, it’s important to understand hip anatomy. The hip is basically a ball-and-socket joint similar to the shoulder joint and the arms. The hip joint is impressive in that it serves two factors, it is a support structure and also very flexible. Because it is a strong support structure, it tends to get injured. Because it’s very flexible, it similarly can be susceptible to injuries.
People routinely have no pain despite the presence of obvious arthritic degeneration, herniated discs, and other seemingly serious structural problems like stenosis and spondylolistheses. This surprising contradiction has been made clear by a wide variety of research over the years, but the most notable in recent history is Brinjikji 2015. There are painful spinal problems, of course — which was also shown by Brinjikji et al in a companion paper — but they are mostly more rare and unpredictable than most people suspect, and there are many fascinating examples of people who “should” be in pain but are not, and vice versa. Spinal problems are only one of many ingredients in back pain. BACK TO TEXT
Pregnancy commonly leads to low back pain by mechanically stressing the lumbar spine (changing the normal lumbar curvature) and by the positioning of the baby inside of the abdomen. Additionally, the effects of the female hormone estrogen and the ligament-loosening hormone relaxin may contribute to loosening of the ligaments and structures of the back. Pelvic-tilt exercises and stretches are often recommended for relieving this pain. Women are also recommended to maintain physical conditioning during pregnancy according to their doctors' advice. Natural labor can also cause low back pain.
^ Jump up to: a b c d e f Qaseem, A; Wilt, TJ; McLean, RM; Forciea, MA; Clinical Guidelines Committee of the American College of, Physicians. (4 April 2017). "Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians". Annals of Internal Medicine. 166 (7): 514–530. doi:10.7326/M16-2367. PMID 28192789.
^ Enke, Oliver; New, Heather A.; New, Charles H.; Mathieson, Stephanie; McLachlan, Andrew J.; Latimer, Jane; Maher, Christopher G.; Lin, C.-W. Christine (2 July 2018). "Anticonvulsants in the treatment of low back pain and lumbar radicular pain: a systematic review and meta-analysis". Canadian Medical Association Journal. 190 (26): E786–E793. doi:10.1503/cmaj.171333. PMC 6028270. PMID 29970367.
Epidural injections of steroid drugs are frequently used to treat sciatica, despite limited evidence for their effectiveness. Moreover, these treatments are based on the assumption that reducing local inflammation in the vertebral column will relieve pain, but an association between structural abnormalities, inflammation, and sciatica symptoms has not been clearly demonstrated. NINDS-funded researchers are using a new imaging technique that can detect inflammation to better understand what causes chronic sciatica pain and to provide evidence to inform treatment selection.



