In the elderly, atherosclerosis can cause weakening of the wall of the large arterial blood vessel (aorta) in the abdomen. This weakening can lead to a bulging (aneurysm) of the aorta wall. While most aneurysms cause no symptoms, some cause a pulsating low back pain. Aneurysms of certain size, especially when enlarging over time, can require surgical repair with a grafting procedure to repair the abnormal portion of the artery.

Everything you need to know about osteoarthritis Osteoarthritis is a potentially painful condition that leads to inflammation, loss of cartilage, and bone damage. Read our article to find out how it happens and what treatments can help. Also, see a fully interactive 3-D model that you can explore to look inside a joint when signs of osteoarthritis begin to appear. Read now
For the 31 million Americans who suffer from daily back pain, relief can be hard to find. In fact, back pain is the single leading cause of disability worldwide and the second most common reason for visits to the doctor. While it can be caused by many different things—extended periods of sitting or standing at work, bad posture, stress, an overly-strenuous workout or helping a friend move, to mention a few—once back pain hits, it can stick around for a long time. Your gut instinct might be to stay frozen until it goes away, but the best thing for your back is to keep it moving with gentle stretches. In fact, a regular routine of a few quick exercises can help you reduce your back pain without a trip to the doctor. Try to do the following exercises every morning and again at night.
In the elderly, atherosclerosis can cause weakening of the wall of the large arterial blood vessel (aorta) in the abdomen. This weakening can lead to a bulging (aneurysm) of the aorta wall. While most aneurysms cause no symptoms, some cause a pulsating low back pain. Aneurysms of certain size, especially when enlarging over time, can require surgical repair with a grafting procedure to repair the abnormal portion of the artery.
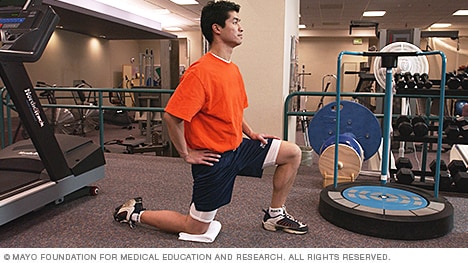
To stretch your quadriceps at the hip, the idea is to do the opposite movement to flexion, i.e., extension. You can perform extension moves at the hip while standing, lying on your side, lying prone (on your stomach) and kneeling. Even basic stretches done at a pain-free level where you can feel a small bit of challenge, and that are held continuously for approximately 30 seconds may translate to better posture and less back pain.
Infection of the discs (septic discitis) and bone (osteomyelitis) is extremely rare. These conditions lead to localized pain associated with fever. The bacteria found when these tissues are tested with laboratory cultures include Staphylococcus aureus and Mycobacterium tuberculosis (TB bacteria). TB infection in the spine is called Pott's disease. These are each very serious conditions requiring long courses of antibiotics. The sacroiliac joints rarely become infected with bacteria. Brucellosis is a bacterial infection that can involve the sacroiliac joints and is usually transmitted in raw goat's milk.
Whether you lift heavy items for your job or simply have a slipped disk from a pesky athletic injury, lower back pain is likely to plague you at some point in your life. Low back pain can result from an acute injury or from chronic overuse that leads to arthritis. This, in turn, can break down the fluid-filled disks in your spine that act as shock absorbers. Whatever the cause, there are some practices you can do to strengthen your back and keep lower back pain at bay.

Brace your core and bend your knees to lower down into a split squat. Your left knee should ideally form a 90-degree angle so that your thigh is parallel to the ground, and your right knee is hovering above the floor. (Quick position check: your left foot should be stepped out far enough that you can do this without letting your left knee go past your left toes—if you can't, hop your left foot out a bit farther away from the bench.)
Marvelously progressive, concise, and cogent guidelines for physicians on the treatment of low back pain. These guidelines almost entirely “get it right” in my opinion, and are completely consistent with recommendations I’ve been making for years on PainScience.com. They are particularly to be praised for strongly discouraging physicians from ordering imaging tests only “for patients with low back pain when severe or progressive neurologic deficits are present or when serious underlying conditions are suspected.”
Some of these red flags are much less red than others, especially depending on the circumstances. For instance, “weight loss” is common and often the sign of successful diet! (Well, at least temporarily successful, anyway. 😃) Obviously, if you know of a harmless reason why you have a red flag symptom, it isn’t really a red flag (duh!). But every single actual red flag — in combination with severe low back pain that’s been going on for several weeks — is definitely a good reason to get yourself checked out.
Epidural steroid injections are most commonly used in situations of radicular pain, which is a radiating pain that is transmitted away from the spine by an irritated spinal nerve. Irritation of a spinal nerve in the low back (lumbar radiculopathy) causes pain that goes down the leg. Epidural injections are also used to treat nerve compression in the neck (cervical spine), referred to as cervical radiculopathy, which causes pain.
Low back pain has been with humans since at least the Bronze Age. The oldest known surgical treatise – the Edwin Smith Papyrus, dating to about 1500 BCE – describes a diagnostic test and treatment for a vertebral sprain. Hippocrates (c. 460 BCE – c. 370 BCE) was the first to use a term for sciatic pain and low back pain; Galen (active mid to late second century CE) described the concept in some detail. Physicians through the end of the first millennium did not attempt back surgery and recommended watchful waiting. Through the Medieval period, folk medicine practitioners provided treatments for back pain based on the belief that it was caused by spirits.[99]

Spinal laminectomy (also known as spinal decompression) is performed when spinal stenosis causes a narrowing of the spinal canal that causes pain, numbness, or weakness. During the procedure, the lamina or bony walls of the vertebrae, along with any bone spurs, are removed. The aim of the procedure is to open up the spinal column to remove pressure on the nerves.
Exercise appears to be useful for preventing low back pain.[47] Exercise is also probably effective in preventing recurrences in those with pain that has lasted more than six weeks.[1][48] Medium-firm mattresses are more beneficial for chronic pain than firm mattresses.[49] There is little to no evidence that back belts are any more helpful in preventing low back pain than education about proper lifting techniques.[47][50] Shoe insoles do not help prevent low back pain.[47][51]

Everything you need to know about osteoarthritis Osteoarthritis is a potentially painful condition that leads to inflammation, loss of cartilage, and bone damage. Read our article to find out how it happens and what treatments can help. Also, see a fully interactive 3-D model that you can explore to look inside a joint when signs of osteoarthritis begin to appear. Read now
Hip labral tear. This is a rip in the ring of cartilage (called the labrum) that follows the outside rim of the socket of your hip joint. Along with cushioning your hip joint, your labrum acts like a rubber seal or gasket to help hold the ball at the top of your thighbone securely within your hip socket. Athletes and people who perform repetitive twisting movements are at higher risk of developing this problem.
The hip flexors are the group of muscles that allow you to lift your knees toward your chest and bend forward from the hips. What is collectively referred to as the hip flexors is actually a group of muscles that includes the iliopsoas, the thigh muscles (rectus femoris, Sartorius and tensor fasciae latae), and the inner thigh muscles (adductor longus and brevis, pectineus and gracilis).
Age: The first attack of low back pain typically occurs between the ages of 30 and 50, and back pain becomes more common with advancing age. As people grow older, loss of bone strength from osteoporosis can lead to fractures, and at the same time, muscle elasticity and tone decrease. The intervertebral discs begin to lose fluid and flexibility with age, which decreases their ability to cushion the vertebrae. The risk of spinal stenosis also increases with age.
Eleven updates have been logged for this article since publication (2009). All PainScience.com updates are logged to show a long term commitment to quality, accuracy, and currency. more When’s the last time you read a blog post and found a list of many changes made to that page since publication? Like good footnotes, this sets PainScience.com apart from other health websites and blogs. Although footnotes are more useful, the update logs are important. They are “fine print,” but more meaningful than most of the comments that most Internet pages waste pixels on.
Don’t medically investigate back pain until it’s met at least three criteria: (1) it’s been bothering you for more than about 6 weeks; (2) it’s severe and/or not improving, or actually getting worse; and (3) there’s at least one other “red flag” (age over 55 or under 20, painful to light tapping, fever/malaise, weight loss, slow urination, incontinence, groin numbness, a dragging toe, or symptoms in both legs like numbness and/or tingling and/or weakness).
Health care professionals diagnose hip pain with a history and physical examination. Physical examination maneuvers, such as internally and externally rotating the hip, can be used to detect pain-aggravating positions. Tenderness can be elicited by palpating over inflamed areas. Straight leg raising can detect signs of sciatica. A health care professional may use imaging studies, including X-rays, CT scans, and MRI scans, to further define the causes of hip pain. Sometimes, nuclear medicine bone scans are used to image inflamed or fractured bone.
^ Jump up to: a b c d e f Qaseem, A; Wilt, TJ; McLean, RM; Forciea, MA; Clinical Guidelines Committee of the American College of, Physicians. (4 April 2017). "Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians". Annals of Internal Medicine. 166 (7): 514–530. doi:10.7326/M16-2367. PMID 28192789.
The medication typically recommended first are NSAIDs (though not aspirin) or skeletal muscle relaxants and these are enough for most people.[13][6] Benefits with NSAIDs; however, is often small.[67] High-quality reviews have found acetaminophen (paracetamol) to be no more effective than placebo at improving pain, quality of life, or function.[68][69] NSAIDs are more effective for acute episodes than acetaminophen; however, they carry a greater risk of side effects including: kidney failure, stomach ulcers and possibly heart problems. Thus, NSAIDs are a second choice to acetaminophen, recommended only when the pain is not handled by the latter. NSAIDs are available in several different classes; there is no evidence to support the use of COX-2 inhibitors over any other class of NSAIDs with respect to benefits.[70][13][71] With respect to safety naproxen may be best.[72] Muscle relaxants may be beneficial.[13]

Pain on the outside of the hip is most commonly due to greater trochanteric bursitis. The greater trochanter is the protrusion where the thigh bone juts outward at the base of the neck (which connects the ball to the femur and is the site of hip stress fractures). A lubricating sac (or bursa) lies over the boney protrusion so that the surrounding muscles do not rub directly on the bone. The top region of the iliotibial (IT) band, known as the tensor fascia lata, is commonly involved in greater trochanteric bursitis.
How to: Lie on your back with your right knee bent and foot flat on the floor (a). With your left leg fully extended, press into your right foot to shift onto your left hip. This is your starting position (b). Then, squeeze your right glutes to press your left hip open until you feel a stretch, pause, then return to start. That’s one rep (c). Perform six to eight reps, then repeat on the opposite side. 
Bone scans are used to detect and monitor infection, fracture, or disorders in the bone. A small amount of radioactive material is injected into the bloodstream and will collect in the bones, particularly in areas with some abnormality. Scanner-generated images can be used to identify specific areas of irregular bone metabolism or abnormal blood flow, as well as to measure levels of joint disease.

The use of lumbar supports in the form of wide elastic bands that can be tightened to provide support to the lower back and abdominal muscles to prevent low back pain remains controversial. Such supports are widely used despite a lack of evidence showing that they actually prevent pain. Multiple studies have determined that the use of lumbar supports provides no benefit in terms of the prevention and treatment of back pain. Although there have been anecdotal case reports of injury reduction among workers using lumbar support belts, many companies that have back belt programs also have training and ergonomic awareness programs. The reported injury reduction may be related to a combination of these or other factors. Furthermore, some caution is advised given that wearing supportive belts may actually lead to or aggravate back pain by causing back muscles to weaken from lack of use.
Meanwhile, many non-dangerous problems can cause amazingly severe back pain. A muscle cramp is a good analogy — just think about how painful a Charley horse is! Regardless of what’s actually going on in there, muscle pain is probably the main thing that back pain patients are feeling. The phenomenon of trigger points — tiny muscle cramps, basically11 — could be the entire problem, or a complication that’s more painful and persistent than the original problem. It’s hard to overstate how painful trigger points can be, but they are not dangerous to anything but your comfort.
Low back pain that lasts at least one day and limits activity is a common complaint.[7] Globally, about 40% of people have LBP at some point in their lives,[7] with estimates as high as 80% of people in the developed world.[22] Approximately 9 to 12% of people (632 million) have LBP at any given point in time, and nearly one quarter (23.2%) report having it at some point over any one-month period.[7][8] Difficulty most often begins between 20 and 40 years of age.[1] Low back pain is more common among people aged 40–80 years, with the overall number of individuals affected expected to increase as the population ages.[7]
Vertebroplasty and kyphoplasty are minimally invasive treatments to repair compression fractures of the vertebrae caused by osteoporosis. Vertebroplasty uses three-dimensional imaging to assist in guiding a fine needle through the skin into the vertebral body, the largest part of the vertebrae. A glue-like bone cement is then injected into the vertebral body space, which quickly hardens to stabilize and strengthen the bone and provide pain relief. In kyphoplasty, prior to injecting the bone cement, a special balloon is inserted and gently inflated to restore height to the vertebral structure and reduce spinal deformity.


