Shingles (herpes zoster) is an acute infection of the nerves that supply sensation to the skin, generally at one or several spinal levels and on one side of the body (right or left). Patients with shingles usually have had chickenpox earlier in life. The herpes virus that causes chickenpox is believed to exist in a dormant state within the spinal nerve roots long after the chickenpox resolves. In people with shingles, this virus reactivates to cause infection along the sensory nerve, leading to nerve pain and usually an outbreak of shingles (tiny blisters on the same side of the body and at the same nerve level). The back pain in patients with shingles of the lumbar area can precede the skin rash by days. Successive crops of tiny blisters can appear for several days and clear with crusty inflammation in one to two weeks. Patients occasionally are left with a more chronic nerve pain (postherpetic neuralgia). Treatment can involve symptomatic relief with lotions, such as calamine, or medications, such as acyclovir (Zovirax), for the infection and pregabalin (Lyrica) or lidocaine (Lidoderm) patches for the pain.

In terms of diagnosing hip pain, typically a patient will expect when they come in to be asked about their symptoms, and it’s very important to find out when did these symptoms start, how long they have been going on, how frequent they are, if they come on in the morning or the evening, do they come on with any certain activity, and if there is something that makes it better or worse. The intensity of the pain is also important. Does it have any associated radiating symptoms? Is it localized in one spot or does it move? After getting a history and finding out what type of pain the patient is having, which also includes whether the pain is dull, aching, sharp, or intense, then it’s important to do a good physical exam. The physical examination involves testing the muscle strength, testing for sensation, doing provocative maneuvers which might help us rule out one type of injury from another.
An injury to a ligament is called a sprain, and an injury to muscle or tendon is called a strain. Sprains and strains may be caused by repetitive movements or a single stressful incident. Symptoms and signs include pain and swelling. Though treatment depends upon the extent and location of the injury, rest, ice, compression, and elevation are key elements of treatment.
You’d think so. But consider this story of a motorcycle accident: many years ago, a friend hit a car that had pulled out from a side street. He flew over the car & landed on his head. Bystanders showed their ignorance of spinal fracture by, yikes, carelessly moving him. In fact, his thoracic spine was significantly fractured … yet the hospital actually refused to do an X-ray because he had no obvious symptoms of a spinal fracture. Incredible! The next day, a horrified orthopedic surgeon ordered an X-ray immediately, confirming the fracture & quite possibly saved him from paralysis.
How to: Stand tall, feet slightly wider than shoulder-width apart, toes pointed out at 45-degree angles (a). Keep your back straight, knees over toes and your weight in the heels of your feet (b). Engage your glutes and thighs as you lower into a deep squat until thighs parallel to the ground (or as close as you can get them) (c). Powering through your heels, push up to return to starting position (d). Repeat. 
Disc degeneration remains a key cause of chronic low back pain and the pain often persists despite surgery. NIH-funded basic science and preclinical studies are investigating molecular-level mechanisms that cause discs in the spine to degenerate, as well as protective mechanisms involved in disc remodeling that may diminish with advancing age. Such studies may help identify future therapeutic strategies to block degenerative mechanisms or promote remodeling processes. NIH also is funding early research on stem cell approaches to promote disc regeneration and rejuvenate cells of the nucleus pulposus, the jelly-like substance in the center of intervertebral discs that loses water content as people age.
^ Enke, Oliver; New, Heather A.; New, Charles H.; Mathieson, Stephanie; McLachlan, Andrew J.; Latimer, Jane; Maher, Christopher G.; Lin, C.-W. Christine (2 July 2018). "Anticonvulsants in the treatment of low back pain and lumbar radicular pain: a systematic review and meta-analysis". Canadian Medical Association Journal. 190 (26): E786–E793. doi:10.1503/cmaj.171333. PMC 6028270. PMID 29970367.
Following any period of prolonged inactivity, a regimen of low-impact exercises is advised. Speed walking, swimming, or stationary bike riding 30 minutes daily can increase muscle strength and flexibility. Yoga also can help stretch and strengthen muscles and improve posture. Consult a physician for a list of low-impact, age-appropriate exercises that are specifically targeted to strengthening lower back and abdominal muscles.
Vertebroplasty and kyphoplasty are minimally invasive treatments to repair compression fractures of the vertebrae caused by osteoporosis. Vertebroplasty uses three-dimensional imaging to assist in guiding a fine needle through the skin into the vertebral body, the largest part of the vertebrae. A glue-like bone cement is then injected into the vertebral body space, which quickly hardens to stabilize and strengthen the bone and provide pain relief. In kyphoplasty, prior to injecting the bone cement, a special balloon is inserted and gently inflated to restore height to the vertebral structure and reduce spinal deformity.
Cancel, pause, or adjust your order at any time, hassle free. Your credit card will only be charged when your order ships. The discount applied every time is 15% off. Since it would be weird to subscribe to a kettlebell, the subscriptions and subscription discounts are only for things you'll need often, like supplements, foods, and personal care items.
Epidural injections of steroid drugs are frequently used to treat sciatica, despite limited evidence for their effectiveness. Moreover, these treatments are based on the assumption that reducing local inflammation in the vertebral column will relieve pain, but an association between structural abnormalities, inflammation, and sciatica symptoms has not been clearly demonstrated. NINDS-funded researchers are using a new imaging technique that can detect inflammation to better understand what causes chronic sciatica pain and to provide evidence to inform treatment selection.

Disk tear. Small tears to the outer part of the disk (annulus) sometimes occur with aging. Some people with disk tears have no pain at all. Others can have pain that lasts for weeks, months, or even longer. A small number of people may develop constant pain that lasts for years and is quite disabling. Why some people have pain and others do not is not well understood.
Injury to the bones and joints: Fractures (breakage of bone) of the lumbar spine and sacrum bone most commonly affect elderly people with osteoporosis, especially those who have taken long-term cortisone medication. For these individuals, occasionally even minimal stresses on the spine (such as bending to tie shoes) can lead to bone fracture. In this setting, the vertebra can collapse (vertebral compression fracture). The fracture causes an immediate onset of severe localized pain that can radiate around the waist in a band-like fashion and is made intensely worse with body motions. This pain generally does not radiate down the lower extremities. Vertebral fractures in younger patients occur only after severe trauma, such as from motor-vehicle accidents or a convulsive seizure.
Don’t medically investigate back pain until it’s met at least three criteria: (1) it’s been bothering you for more than about 6 weeks; (2) it’s severe and/or not improving, or actually getting worse; and (3) there’s at least one other “red flag” (age over 55 or under 20, painful to light tapping, fever/malaise, weight loss, slow urination, incontinence, groin numbness, a dragging toe, or symptoms in both legs like numbness and/or tingling and/or weakness).
Hip pain and stiffness is a common condition treated at Airrosti. The hip is one of the largest joints in the body. To function correctly and with full range of motion, the ligaments, muscles, and fascia surrounding the joint must be working in unison. Our providers are trained to find the source of the pain and eliminate it quickly and safely — typically in as few as three visits based on patient-reported outcomes.
Low back pain can be caused by tumors, either benign or malignant, that originate in the bone of the spine or pelvis and spinal cord (primary tumors) and those which originate elsewhere and spread to these areas (metastatic tumors). Symptoms range from localized pain to radiating severe pain and loss of nerve and muscle function (even incontinence of urine and stool) depending on whether or not the tumors affect the nervous tissue. Tumors of these areas are detected using imaging tests, such as plain X-rays, nuclear bone scanning, and CAT and MRI scanning.
Exercise therapy is effective in decreasing pain and improving function for those with chronic low back pain.[50] It also appears to reduce recurrence rates for as long as six months after the completion of program[61] and improves long-term function.[57] There is no evidence that one particular type of exercise therapy is more effective than another.[62] The Alexander technique appears useful for chronic back pain,[63] and there is tentative evidence to support the use of yoga.[64] Transcutaneous electrical nerve stimulation (TENS) has not been found to be effective in chronic low back pain.[65] Evidence for the use of shoe insoles as a treatment is inconclusive.[51] Peripheral nerve stimulation, a minimally-invasive procedure, may be useful in cases of chronic low back pain that do not respond to other measures, although the evidence supporting it is not conclusive, and it is not effective for pain that radiates into the leg.[66]

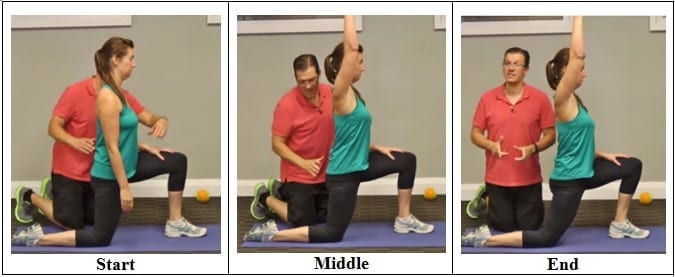
Prolonged sitting and activities like running or cycling can lead to tight hip flexor muscles and a variety of skeletal imbalances. Think: if you only cycle for exercise, certain muscles in your legs will get stronger (in a lot of cases you overwork these muscles) yet your core and outer hip muscles might get weaker from lack of engagement. So what? Well, these muscle imbalances often lead to skeletal imbalances and injuries down the line. If you have particularly tight hip flexors, your body will start to create an anterior pull on the pelvis (anterior pelvic tilt). You can identify an anterior pelvic tilt if your belly protrudes slightly in the front while your butt sticks out in the back (what some people refer to as “duck butt”).
The site navigation utilizes arrow, enter, escape, and space bar key commands. Left and right arrows move across top level links and expand / close menus in sub levels. Up and Down arrows will open main level menus and toggle through sub tier links. Enter and space open menus and escape closes them as well. Tab will move on to the next part of the site rather than go through menu items.

Biofeedback is used to treat many acute pain problems, most notably back pain and headache. The therapy involves the attachment of electrodes to the skin and the use of an electromyography machine that allows people to become aware of and selfregulate their breathing, muscle tension, heart rate, and skin temperature. People regulate their response to pain by using relaxation techniques. Biofeedback is often used in combination with other treatment methods, generally without side effects. Evidence is lacking that biofeedback provides a clear benefit for low back pain.
5. Feel free as a bird. Open up those hips with yoga’s pigeon pose! Start on all fours with hands below the shoulders and knees below the hips. Bring the right knee forward until it touches the right hand and place the leg flat on the ground across the body (the right foot is now on the left side of the body, parallel to the front of the mat). Drop left leg to the ground, and extend it back with toes turned under. Keep the hips level, inhale, and walk hands forward. Exhale, and fold the torso over, lowering elbows to the floor. Stay in this position for 5-10 breaths before coming back up to switch sides.