^ Jump up to: a b c d American College of Occupational and Environmental Medicine (February 2014), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, American College of Occupational and Environmental Medicine, archived from the original on 11 September 2014, retrieved 24 February 2014, which cites
Putting the exercise in writing do not help me, I need to watch them doing them so, I can figer out how to do them, or if I should even try to do them. I use the flex extendors, lifting my legs one at a time from the flor to strengthen my thys, hip and buttox. And I try to remember to do the bridge excerise. I have had 2 total hip replacements , 7 months a part, in 2013. Trying to get stronger with cold weather will be 70 in Feb. Linda
Running: Running may be good for boosting your cardiovascular health but it can be very strenuous if you have hip pain. The impact can upset your hip joints so instead focus on other forms of exercise. Walking is still a good option for hip pain if you really feel like working out in the great outdoors or you could instead try some strengthening exercises from the comfort of your own home.

Paget's disease of the bone is a condition of unknown cause in which the bone formation is out of synchrony with normal bone remodeling. This condition results in abnormally weakened bone and deformity and can cause localized bone pain, though it often causes no symptoms. Paget's disease is more common in people over the age of 50. Heredity (genetic background) and certain unusual virus infections have been suggested as causes. Thickening of involved bony areas of the lumbar spine can cause the radiating lower extremity pain of sciatica.
Why is back pain still a huge problem? Maybe this: “It is extremely difficult to alter the potentially disabling belief among the lay public that low back pain has a structural mechanical cause. An important reason for this is that this belief continues to be regularly reinforced by the conditions of care of a range of ‘hands-on’ providers, for whom idiosyncratic variations of that view are fundamental to their professional existence.”

Spinal manipulation and spinal mobilization are approaches in which professionally licensed specialists (doctors of chiropractic care) use their hands to mobilize, adjust, massage, or stimulate the spine and the surrounding tissues. Manipulation involves a rapid movement over which the individual has no control; mobilization involves slower adjustment movements. The techniques have been shown to provide small to moderate short-term benefits in people with chronic low back pain. Evidence supporting their use for acute or subacute low back pain is generally of low quality. Neither technique is appropriate when a person has an underlying medical cause for the back pain such as osteoporosis, spinal cord compression, or arthritis.
Meanwhile, many non-dangerous problems can cause amazingly severe back pain. A muscle cramp is a good analogy — just think about how painful a Charley horse is! Regardless of what’s actually going on in there, muscle pain is probably the main thing that back pain patients are feeling. The phenomenon of trigger points — tiny muscle cramps, basically11 — could be the entire problem, or a complication that’s more painful and persistent than the original problem. It’s hard to overstate how painful trigger points can be, but they are not dangerous to anything but your comfort.
^ Coxib and traditional NSAID Trialists' (CNT) Collaboration, Bhala N, Emberson J, Merhi A, Abramson S, Arber N, Baron JA, Bombardier C, Cannon C, Farkouh ME, FitzGerald GA, Goss P, Halls H, Hawk E, Hawkey C, Hennekens C, Hochberg M, Holland LE, Kearney PM, Laine L, Lanas A, Lance P, Laupacis A, Oates J, Patrono C, Schnitzer TJ, Solomon S, Tugwell P, Wilson K, Wittes J, Baigent C (Aug 31, 2013). "Vascular and upper gastrointestinal effects of non-steroidal anti-inflammatory drugs: meta-analyses of individual participant data from randomised trials". Lancet. 382 (9894): 769–79. doi:10.1016/S0140-6736(13)60900-9. PMC 3778977. PMID 23726390.
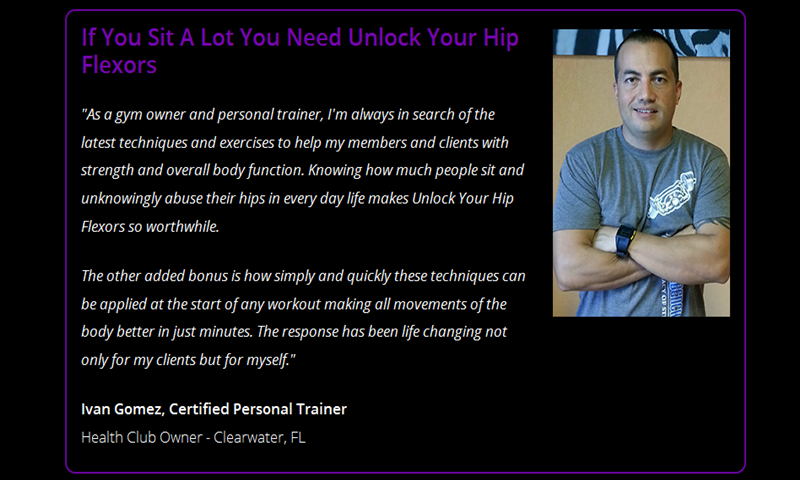
With the stakes so high, doesn’t it make sense to do all you can to strengthen and protect your hips? Even if you have arthritis in a hip — the reason for 8 in 10 replacements — you may be able to manage pain with exercise. In a 2017 pilot study published in the Journal of Osteoporosis, women 65 and older who exercised three times a week in a supervised 12-week program reduced arthritic hip pain by over 30 percent, with similar gains in strength, and joint range of motion. The four exercises here will fortify the muscles that surround and support your hips, says trainer Robert Linkul, owner of Be Stronger Fitness in Sacramento, Calif. He advises doing these simple moves, two to three sets of five to 10 reps each, three times a week. Compare how you feel after three weeks.
The magnitude of the burden from low back pain has grown worse in recent years. In 1990, a study ranking the most burdensome conditions in the U.S. in terms of mortality or poor health as a result of disease put low back pain in sixth place; in 2010, low back pain jumped to third place, with only ischemic heart disease and chronic obstructive pulmonary disease ranking higher.
Veritas Health publishes original and accessible health related content written by more than 100 physician authors and peer-reviewed by a 16 member Medical Advisory Board. The Veritas Health platform comprising of Spine-health.com, Arthritis-health.com, Sports-health.com, and Pain-health.com, provides comprehensive information on back pain, arthritis, sports injuries, and chronic pain conditions. For more information visit Veritashealth.com.
The AANS does not endorse any treatments, procedures, products or physicians referenced in these patient fact sheets. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific neurosurgical advice or assistance should consult his or her neurosurgeon, or locate one in your area through the AANS’ Find a Board-certified Neurosurgeon” online tool.
Veritas Health publishes original and accessible health related content written by more than 100 physician authors and peer-reviewed by a 16 member Medical Advisory Board. The Veritas Health platform comprising of Spine-health.com, Arthritis-health.com, Sports-health.com, and Pain-health.com, provides comprehensive information on back pain, arthritis, sports injuries, and chronic pain conditions. For more information visit Veritashealth.com.
Blood tests are not routinely used to diagnose the cause of back pain; however in some cases they may be ordered to look for indications of inflammation, infection, and/or the presence of arthritis. Potential tests include complete blood count, erythrocyte sedimentation rate, and C-reactive protein. Blood tests may also detect HLA-B27, a genetic marker in the blood that is more common in people with ankylosing spondylitis or reactive arthritis (a form of arthritis that occurs following infection in another part of the body, usually the genitourinary tract).
Blood tests are not routinely used to diagnose the cause of back pain; however in some cases they may be ordered to look for indications of inflammation, infection, and/or the presence of arthritis. Potential tests include complete blood count, erythrocyte sedimentation rate, and C-reactive protein. Blood tests may also detect HLA-B27, a genetic marker in the blood that is more common in people with ankylosing spondylitis or reactive arthritis (a form of arthritis that occurs following infection in another part of the body, usually the genitourinary tract).
Arthritis: The spondyloarthropathies are inflammatory types of arthritis that can affect the lower back and sacroiliac joints. Examples of spondyloarthropathies include reactive arthritis (Reiter's disease), ankylosing spondylitis, psoriatic arthritis, and the arthritis of inflammatory bowel disease. Each of these diseases can lead to low back pain and stiffness, which is typically worse in the morning. These conditions usually begin in the second and third decades of life. They are treated with medications directed toward decreasing the inflammation. Newer biologic medications have been greatly successful in both quieting the disease and stopping its progression.

Apply the above concept to your hips. When you sit, your hips are in a "flexed" position. Therefore, the muscles that flex your hips are in a shortened state. You probably spend at least a third of your day sitting down. Think about how much time those hip flexor muscles stay shortened. A lot. Over time, they become tighter and tighter until you look like the old man in the picture. So unless you want to look like that, perform the stretches shown below.

To help you strengthen these important muscles, Miranda put together a list of exercises, below. They include dynamic warm-up moves, meant to activate your hip muscles and prep them for the bigger movements to come; functional moves that train basic movement patterns, like the squat, hip hinge, and lunge; functional plyometric exercises that train explosive power; and a few moves that get you moving in different planes of motion, or directions.
Why is back pain still a huge problem? Maybe this: “It is extremely difficult to alter the potentially disabling belief among the lay public that low back pain has a structural mechanical cause. An important reason for this is that this belief continues to be regularly reinforced by the conditions of care of a range of ‘hands-on’ providers, for whom idiosyncratic variations of that view are fundamental to their professional existence.”
Veritas Health publishes original and accessible health related content written by more than 100 physician authors and peer-reviewed by a 16 member Medical Advisory Board. The Veritas Health platform comprising of Spine-health.com, Arthritis-health.com, Sports-health.com, and Pain-health.com, provides comprehensive information on back pain, arthritis, sports injuries, and chronic pain conditions. For more information visit Veritashealth.com.
The hip joint is designed to withstand a fair amount of wear and tear, but it’s not indestructible. For example, when you walk, a cushion of cartilage helps prevent friction as the hip bone moves in its socket. With age and use, this cartilage can wear down or become damaged, or the hip bone itself can be fractured during a fall. In fact, more than 300,000 adults over 65 are hospitalized for hip fractures each year, according to the Agency for Healthcare Research and Quality.
Stop focusing on a specific diagnosis. Up to 85% of low back pain can be classified as "non-specific." This means that the origin of your pain cannot be localized to one specific structure or problem. While common diagnostic tests for low back pain can show the bones, discs, and joints with great detail, no test can tell the exact cause of your pain with 100% accuracy.

Several NIH-funded clinical trials and other studies in patients aim to improve treatment options and prevention strategies for chronic low back pain, as well as add to the evidence base about existing treatments. A multi-year multicenter study called the Spine Patient Outcomes Research Trial (SPORT) compared the most commonly used surgical and nonsurgical treatments for patients with the three most common diagnoses for which spine surgery is performed: intervertebral disc herniation, spinal stenosis, and degenerative spondylisthesis. SPORT represented the largest clinical investigation to date looking at treatment results for these disabling and costly causes of chronic low back pain.
Nerve irritation: The nerves of the lumbar spine can be irritated by mechanical pressure (impingement) by bone or other tissues, or from disease, anywhere along their paths -- from their roots at the spinal cord to the skin surface. These conditions include lumbar disc disease (radiculopathy), bony encroachment, and inflammation of the nerves caused by a viral infection (shingles). See descriptions of these conditions below. 
The presence of certain signs, termed red flags, indicate the need for further testing to look for more serious underlying problems, which may require immediate or specific treatment.[5][36] The presence of a red flag does not mean that there is a significant problem. It is only suggestive,[37][38] and most people with red flags have no serious underlying problem.[3][1] If no red flags are present, performing diagnostic imaging or laboratory testing in the first four weeks after the start of the symptoms has not been shown to be useful.[5]
Backpack overload in children: Low back pain unrelated to injury or other known cause is unusual in pre-teen children. However, a backpack overloaded with schoolbooks and supplies can strain the back and cause muscle fatigue. The American Academy of Orthopaedic Surgeons recommends that a child’s backpack should weigh no more than 15 to 20 percent of the child’s body weight.
Bone scans are used to detect and monitor infection, fracture, or disorders in the bone. A small amount of radioactive material is injected into the bloodstream and will collect in the bones, particularly in areas with some abnormality. Scanner-generated images can be used to identify specific areas of irregular bone metabolism or abnormal blood flow, as well as to measure levels of joint disease.

Strong muscles support and protect your joints. “Strengthening the lower body takes some of the pressure off of the hip and knee joints,” says William Oswald, DPT, a physical therapist and clinical instructor of rehabilitation medicine at NYU Langone Health. This can relieve some of the pain and protect against more damage. “It can also make daily tasks, such as climbing the stairs, easier,” he says.

From a physical therapist’s perspective, these are excellent exercises for lower back pain (LBP) resulting from muscular tightness or stiff joints. However, LBP can also be caused by bulging (or “herniated”) discs, pinched nerves, and the like. If your LBP worsens (or radiates into your leg) upon attempting these or any other low back exercises, you should seek medical attention. Physical therapists are musculoskeletal experts that are able to properly evaluate and treat your back pain symptoms. And, according to a recently passed law in the state of Michigan, a physician referral is no longer necessary to seek treatment from a physical therapist. So, if you are experiencing LBP that is not improving…#getPT!

How to: Lie on your back with your right knee bent and foot flat on the floor (a). With your left leg fully extended, press into your right foot to shift onto your left hip. This is your starting position (b). Then, squeeze your right glutes to press your left hip open until you feel a stretch, pause, then return to start. That’s one rep (c). Perform six to eight reps, then repeat on the opposite side.
I am a science writer, former massage therapist, and I was the assistant editor at ScienceBasedMedicine.org for several years. I have had my share of injuries and pain challenges as a runner and ultimate player. My wife and I live in downtown Vancouver, Canada. See my full bio and qualifications, or my blog, Writerly. You might run into me on Facebook or Twitter.
Knowing the exact source of your hip pain can provide you with peace of mind—but receiving the right treatment is even better. Let Dr. Hamilton provide you with both peace of mind and relief from your symptoms. Schedule an appointment with Dr. Hamilton today. For your convenience, he is available at Beacon East, Beacon West, or Summit Woods in Ohio as well as Beacon’s Northern Kentucky location.
Intervertebral disc degeneration is one of the most common mechanical causes of low back pain, and it occurs when the usually rubbery discs lose integrity as a normal process of aging. In a healthy back, intervertebral discs provide height and allow bending, flexion, and torsion of the lower back. As the discs deteriorate, they lose their cushioning ability.
Start in a runner’s lunge with right leg forward, right knee over right ankle and back leg straight. Walk right foot over toward left hand, then drop right shin and thigh to the floor, making sure to keep right knee in line with right hip. Allow left leg to rest on the floor with top of left foot facing down. Take a moment to square your hips to the front of the room. Hold here, or hinge at hips and lower torso toward floor, allowing head to rest on forearms. Hold for at least 30 seconds, then repeat on opposite side. You want to feel a moderate stretch in the outside of the right thigh, but if this pose hurts your knees or feels too uncomfortable, stick with Thread the Needle.

Degenerative bone and joint conditions: As we age, the water and protein content of the body's cartilage changes. This change results in weaker, thinner, and more fragile cartilage. Because both the discs and the joints that stack the vertebrae (facet joints) are partly composed of cartilage, these areas are subject to wear and tear over time (degenerative changes). Degeneration of the disc is called spondylosis. Spondylosis can be noted on X-rays of the spine as a narrowing of the normal "disc space" between the vertebrae. It is the deterioration of the disc tissue that predisposes the disc to herniation and localized lumbar pain ("lumbago") in older patients. Degenerative arthritis (osteoarthritis) of the facet joints is also a cause of localized lumbar pain that can be detected with plain X-ray testing. These causes of degenerative back pain are usually treated conservatively with intermittent heat, rest, rehabilitative exercises, and medications to relieve pain, muscle spasm, and inflammation.
You could do these moves all together as a single workout, or, as Miranda suggests, split them in half and do the first part one day and the second part another—"but do the warm-up with each one," she says. Those first three moves are meant to not only "wake up" the muscles, but also get your brain ready for the movement patterns to come. For that reason, she says that doing the first three moves "would be a fantastic warm-up before any workout."

The magnitude of the burden from low back pain has grown worse in recent years. In 1990, a study ranking the most burdensome conditions in the U.S. in terms of mortality or poor health as a result of disease put low back pain in sixth place; in 2010, low back pain jumped to third place, with only ischemic heart disease and chronic obstructive pulmonary disease ranking higher.
Arthritis: The spondyloarthropathies are inflammatory types of arthritis that can affect the lower back and sacroiliac joints. Examples of spondyloarthropathies include reactive arthritis (Reiter's disease), ankylosing spondylitis, psoriatic arthritis, and the arthritis of inflammatory bowel disease. Each of these diseases can lead to low back pain and stiffness, which is typically worse in the morning. These conditions usually begin in the second and third decades of life. They are treated with medications directed toward decreasing the inflammation. Newer biologic medications have been greatly successful in both quieting the disease and stopping its progression.
You could do these moves all together as a single workout, or, as Miranda suggests, split them in half and do the first part one day and the second part another—"but do the warm-up with each one," she says. Those first three moves are meant to not only "wake up" the muscles, but also get your brain ready for the movement patterns to come. For that reason, she says that doing the first three moves "would be a fantastic warm-up before any workout."
Sit in a chair with good lumbar support and proper position and height for the task. Keep shoulders back. Switch sitting positions often and periodically walk around the office or gently stretch muscles to relieve tension. A pillow or rolled-up towel placed behind the small of the back can provide some lumbar support. During prolonged periods of sitting, elevate feet on a low stool or a stack of books.

Exercise therapy is effective in decreasing pain and improving function for those with chronic low back pain.[50] It also appears to reduce recurrence rates for as long as six months after the completion of program[61] and improves long-term function.[57] There is no evidence that one particular type of exercise therapy is more effective than another.[62] The Alexander technique appears useful for chronic back pain,[63] and there is tentative evidence to support the use of yoga.[64] Transcutaneous electrical nerve stimulation (TENS) has not been found to be effective in chronic low back pain.[65] Evidence for the use of shoe insoles as a treatment is inconclusive.[51] Peripheral nerve stimulation, a minimally-invasive procedure, may be useful in cases of chronic low back pain that do not respond to other measures, although the evidence supporting it is not conclusive, and it is not effective for pain that radiates into the leg.[66]

Pain in the hip can result from a number of factors. Sometimes diseases that affect other joints in the body, such as the inflammation resulting from arthritis, can be the cause of pain in the hip. Depending upon the cause of hip pain, the pain may occur when walking, running, or engaging in activity. Trochanteric bursitis is the most common type of hip bursitis and causes pain at the point of the hip.
If low back pain gets worse or does not improve after two to three days of home treatment, contact a primary-care physician. The physician can evaluate the patient and perform a neurological exam in the office to determine which nerve root is being irritated, as well as rule out other serious medical conditions. If there are clear signs that the nerve root is being compressed, a physician can prescribe medications to relieve the pain, swelling and irritation; he or she also may recommend limitation of activities. If these treatment options do not provide relief within two weeks, it may be time to consider other diagnostic studies and possibly surgery.


