Disc degeneration remains a key cause of chronic low back pain and the pain often persists despite surgery. NIH-funded basic science and preclinical studies are investigating molecular-level mechanisms that cause discs in the spine to degenerate, as well as protective mechanisms involved in disc remodeling that may diminish with advancing age. Such studies may help identify future therapeutic strategies to block degenerative mechanisms or promote remodeling processes. NIH also is funding early research on stem cell approaches to promote disc regeneration and rejuvenate cells of the nucleus pulposus, the jelly-like substance in the center of intervertebral discs that loses water content as people age.

When you're working to strengthen the core, you'll want to focus on exercises that don't exacerbate lower back issues. "It's important to find out which movements (flexion, extension, rotation) cause pain or discomfort and to avoid those movements, while continuing to work into ranges that are not provoking," Dircksen says. Crockford suggests focusing on exercises that keep the core stable and avoiding twisting movements to avoid exacerbating pain.
The medication typically recommended first are NSAIDs (though not aspirin) or skeletal muscle relaxants and these are enough for most people.[13][6] Benefits with NSAIDs; however, is often small.[67] High-quality reviews have found acetaminophen (paracetamol) to be no more effective than placebo at improving pain, quality of life, or function.[68][69] NSAIDs are more effective for acute episodes than acetaminophen; however, they carry a greater risk of side effects including: kidney failure, stomach ulcers and possibly heart problems. Thus, NSAIDs are a second choice to acetaminophen, recommended only when the pain is not handled by the latter. NSAIDs are available in several different classes; there is no evidence to support the use of COX-2 inhibitors over any other class of NSAIDs with respect to benefits.[70][13][71] With respect to safety naproxen may be best.[72] Muscle relaxants may be beneficial.[13]

Exercise therapy is effective in decreasing pain and improving function for those with chronic low back pain.[50] It also appears to reduce recurrence rates for as long as six months after the completion of program[61] and improves long-term function.[57] There is no evidence that one particular type of exercise therapy is more effective than another.[62] The Alexander technique appears useful for chronic back pain,[63] and there is tentative evidence to support the use of yoga.[64] Transcutaneous electrical nerve stimulation (TENS) has not been found to be effective in chronic low back pain.[65] Evidence for the use of shoe insoles as a treatment is inconclusive.[51] Peripheral nerve stimulation, a minimally-invasive procedure, may be useful in cases of chronic low back pain that do not respond to other measures, although the evidence supporting it is not conclusive, and it is not effective for pain that radiates into the leg.[66]
Stretching is your next move, but not just any stretches. “Before your workout, you want to go for dynamic stretches, or stretches that put the joint through a full range of motion,” says Lefkowith. Moves like squats and lunges will get your muscles fired up (especially if you focus on squeezing your butt at the top of those squats), says Lefkowith.
Along with these exercises, it's also important to do some supplementary exercises to work your hip's supporting muscles. You've probably heard of your shoulder's rotator cuff. Well, your hip also has a cuff, or a group of muscles that help stabilize and support movement. For these exercises, you'll need a mini-band, a longer thera-band or tubing (both are sold at many sporting goods stores, or can be purchased online), and a cable-column unit.
As the structure of the back is complex and the reporting of pain is subjective and affected by social factors, the diagnosis of low back pain is not straightforward.[5] While most low back pain is caused by muscle and joint problems, this cause must be separated from neurological problems, spinal tumors, fracture of the spine, and infections, among others.[3][1]
Massage therapy does not appear to provide much benefit for acute low back pain.[1] A 2015 Cochrane review found that for acute low back pain massage therapy was better than no treatment for pain only in the short-term.[89] There was no effect for improving function.[89] For chronic low back pain massage therapy was no better than no treatment for both pain and function, though only in the short-term.[89] The overall quality of the evidence was low and the authors conclude that massage therapy is generally not an effective treatment for low back pain.[89]

^ Enke, Oliver; New, Heather A.; New, Charles H.; Mathieson, Stephanie; McLachlan, Andrew J.; Latimer, Jane; Maher, Christopher G.; Lin, C.-W. Christine (2 July 2018). "Anticonvulsants in the treatment of low back pain and lumbar radicular pain: a systematic review and meta-analysis". Canadian Medical Association Journal. 190 (26): E786–E793. doi:10.1503/cmaj.171333. PMC 6028270. PMID 29970367.

When you tell your doctor your hip hurts, the first thing she should do is confirm that your hip is actually the problem. Women might say they have hip pain, but what they may mean is that they have pain in the side of the upper thigh or upper buttock, or they may be experiencing lower back pain, says Stephanie E. Siegrist, MD, an orthopedic surgeon in Rochester, New York, and a spokeswoman for the American Academy of Orthopaedic Surgeons. Hip pain is often felt in the groin or on the outside of the hip directly over where the hip joint (a ball-and-socket joint) is located.
Kneel on your mat with thighs perpendicular to the floor and tops of of your feet facing down. Place a yoga block between your feet. Bring your inner knees together. Slide your feet apart so they are slightly wider than your hips, and press the tops of your feet evenly into the mat. Slowly sit down on the yoga block. Use your hands to turn the top of your thighs inward. Allow the backs of your hands to rest on your thighs. Hold for at least 30 seconds.
Lumbar strain (acute, chronic): A lumbar strain is a stretch injury to the ligaments, tendons, and/or muscles of the low back. The stretching incident results in microscopic tears of varying degrees in these tissues. Lumbar strain is considered one of the most common causes of low back pain. The injury can occur because of overuse, improper use, or trauma. Soft-tissue injury is commonly classified as "acute" if it has been present for days to weeks. If the strain lasts longer than three months, it is referred to as "chronic." Lumbar strain most often occurs in people in their 40s, but it can happen at any age. The condition is characterized by localized discomfort in the low back area with onset after an event that mechanically stressed the lumbar tissues. The severity of the injury ranges from mild to severe, depending on the degree of strain and resulting spasm of the muscles of the low back. The diagnosis of lumbar strain is based on the history of injury, the location of the pain, and exclusion of nervous system injury. Usually, X-ray testing is only helpful to exclude bone abnormalities.
Following any period of prolonged inactivity, a regimen of low-impact exercises is advised. Speed walking, swimming, or stationary bike riding 30 minutes daily can increase muscle strength and flexibility. Yoga also can help stretch and strengthen muscles and improve posture. Consult a physician for a list of low-impact, age-appropriate exercises that are specifically targeted to strengthening lower back and abdominal muscles.


The vast majority of low back pain is mechanical in nature. In many cases, low back pain is associated with spondylosis, a term that refers to the general degeneration of the spine associated with normal wear and tear that occurs in the joints, discs, and bones of the spine as people get older. Some examples of mechanical causes of low back pain include:
Grade II (moderate): A larger tear in your muscle that makes it difficult to move and causes a moderate amount of pain, especially when you move the affected muscle, swelling, and tenderness. You may have 5 percent to 50 percent loss of function and you may be limping. You can't go back to sporting activities until the tear is completely healed. These injuries can take anywhere from a couple weeks to a few months to heal, depending on how bad they are.
Spondylolisthesis. This condition occurs when one vertebra slips over the adjacent one. There are 5 types of spondylolisthesis but the most common are secondary to a defect or fracture of the pars (between the facet joints) or mechanical instability of the facet joints (degenerative). The pain can be caused by instability (back) or compression of the nerves (leg).

Hip hikers (also known as the pelvic drop) are great exercises to get your gluteal muscles working in a weight bearing position. To do the exercise, stand sideways with one foot on a step and the other hanging off. Keeping both knees straight, lower down your pelvis on one side so your foot moves toward the floor. Both knees should remain straight; the motion should come from your hip joint. Once your pelvis is lowered down, slowly raise it back up to the starting position. Repeat the exercise for 10 repetitions.
Really a great content. Let me tell you first about hip flexor it is the engine through which our body moves. They control balance, our ability to sit, stand, twist, reach, bend, walk and step. One of my patient also suffering from same problem but due to lack of money he was unable to afford a treatment. So i recommend him a program to unlock hip flexor. If anyone wants they can check it out here ;- https://tinyurl.com/y8yaqs2s Report
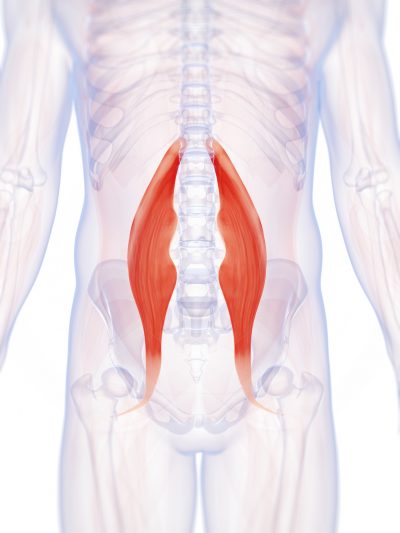
Really a great content. Let me tell you first about hip flexor it is the engine through which our body moves. They control balance, our ability to sit, stand, twist, reach, bend, walk and step. One of my patient also suffering from same problem but due to lack of money he was unable to afford a treatment. So i recommend him a program to unlock hip flexor. If anyone wants they can check it out here ;- https://tinyurl.com/y8yaqs2s Report
Note: Exercises that strengthen the hip flexors also involve contracting (shortening) these muscles. So if tight hip flexors are a problem for you, it might be wise to limit how many direct hip-strengthening exercises you perform. These exercises are more geared toward people who have been told they have weak hip flexors that need strengthening or are looking for targeted exercises to build more power and stamina in the hip flexors.
But moving is important for hip and knee OA. It causes your joints to compress and release, bringing blood flow, nutrients, and oxygen into the cartilage. “This can help prolong the function and longevity of your joints,” says Eric Robertson, DPT, a physical therapist and associate professor of clinical physical therapy at the University of Southern California.

Workers who experience acute low back pain as a result of a work injury may be asked by their employers to have x-rays.[102] As in other cases, testing is not indicated unless red flags are present.[102] An employer's concern about legal liability is not a medical indication and should not be used to justify medical testing when it is not indicated.[102] There should be no legal reason for encouraging people to have tests which a health care provider determines are not indicated.[102]
Hip bursitis — an inflammation between your thighbone and nearby tendons — is commonly diagnosed when patients have pain on the outer side of the hip. However, several other conditions can cause similar pain, and require different treatments. "Doctors often assume that pain on the outer side of the hip is due to bursitis. But 90% of the time, it's not bursitis," says Dr. Lauren Elson, a physiatrist with Harvard-affiliated Massachusetts General Hospital.
Exercise therapy is effective in decreasing pain and improving function for those with chronic low back pain.[50] It also appears to reduce recurrence rates for as long as six months after the completion of program[61] and improves long-term function.[57] There is no evidence that one particular type of exercise therapy is more effective than another.[62] The Alexander technique appears useful for chronic back pain,[63] and there is tentative evidence to support the use of yoga.[64] Transcutaneous electrical nerve stimulation (TENS) has not been found to be effective in chronic low back pain.[65] Evidence for the use of shoe insoles as a treatment is inconclusive.[51] Peripheral nerve stimulation, a minimally-invasive procedure, may be useful in cases of chronic low back pain that do not respond to other measures, although the evidence supporting it is not conclusive, and it is not effective for pain that radiates into the leg.[66]
Meanwhile, it’s extremely common for non-life-threatening low back pain to be alarmingly severe and persistent — to have a loud bark! Your doctor may not appreciate how true this is, and may over-react to all persistent low back pain, even without other red flags. In most cases, you shouldn’t let them scare you. Being “freaked out” about persistent back pain is the real threat: it can make low back pain much worse, and much more likely to last even longer (a tragic irony).

Meanwhile, it’s extremely common for non-life-threatening low back pain to be alarmingly severe and persistent — to have a loud bark! Your doctor may not appreciate how true this is, and may over-react to all persistent low back pain, even without other red flags. In most cases, you shouldn’t let them scare you. Being “freaked out” about persistent back pain is the real threat: it can make low back pain much worse, and much more likely to last even longer (a tragic irony).

If low back pain gets worse or does not improve after two to three days of home treatment, contact a primary-care physician. The physician can evaluate the patient and perform a neurological exam in the office to determine which nerve root is being irritated, as well as rule out other serious medical conditions. If there are clear signs that the nerve root is being compressed, a physician can prescribe medications to relieve the pain, swelling and irritation; he or she also may recommend limitation of activities. If these treatment options do not provide relief within two weeks, it may be time to consider other diagnostic studies and possibly surgery.


