Shingles (herpes zoster) is an acute infection of the nerves that supply sensation to the skin, generally at one or several spinal levels and on one side of the body (right or left). Patients with shingles usually have had chickenpox earlier in life. The herpes virus that causes chickenpox is believed to exist in a dormant state within the spinal nerve roots long after the chickenpox resolves. In people with shingles, this virus reactivates to cause infection along the sensory nerve, leading to nerve pain and usually an outbreak of shingles (tiny blisters on the same side of the body and at the same nerve level). The back pain in patients with shingles of the lumbar area can precede the skin rash by days. Successive crops of tiny blisters can appear for several days and clear with crusty inflammation in one to two weeks. Patients occasionally are left with a more chronic nerve pain (postherpetic neuralgia). Treatment can involve symptomatic relief with lotions, such as calamine, or medications, such as acyclovir (Zovirax), for the infection and pregabalin (Lyrica) or lidocaine (Lidoderm) patches for the pain.

To help you strengthen these important muscles, Miranda put together a list of exercises, below. They include dynamic warm-up moves, meant to activate your hip muscles and prep them for the bigger movements to come; functional moves that train basic movement patterns, like the squat, hip hinge, and lunge; functional plyometric exercises that train explosive power; and a few moves that get you moving in different planes of motion, or directions.
Like quadriceps, the hamstrings are 2-joint muscles. Unlike the quadriceps, though, the hamstrings reside at the back of your thigh. They attach at the siting bones, which are located on the underside of your pelvis. When the hamstring muscles contract, the effect is a pulling of the back of the pelvis down toward the back of the thigh, or a bringing of the lower extremity back behind you.
Squats. Using a squat machine will strengthen your quadriceps muscles on the front of your thigh and the hamstring muscles on the back of your thigh, both of which attach to your hip and give it support. The squat machine may be vertical, in which case you’ll start in a standing position and bend your knees until your thighs are parallel to the floor, or it may be on a sliding incline board.
In addition to strengthening the core muscles, it's also important to address any mobility problems, says Jacque Crockford, M.S., C.S.C.S., exercise physiology content manager at American Council on Exercise, which can sometimes be what's causing pain. If specific movements like twisting or bending or extending your spine feel uncomfortable, there may be mobility (flexibility) issues at play. Doing some gentle stretching (like these yoga poses) might help. (If it gets worse with those stretches, stop and see a doctor.)

As has been highlighted by research presented at the national meeting of the American College of Rheumatology, a very important aspect of the individual evaluation is the patient's own understanding and perception of their particular situation. British researchers found that those who believed that their symptoms had serious consequences on their lives and that they had, or treatments had, little control over their symptoms were more likely to have a poor outcome. This research points out to physicians the importance of addressing the concerns and perceptions that patients have about their condition during the initial evaluations.
People understandably assume that the worst back pain is the scariest. In fact, pain intensity is a poor indicator of back pain ominousness,10 and some of the worst causes are actually the least painful (especially in the early stages). For instance, someone could experience the symptoms of cauda equinae syndrome, and be in real danger of a serious and permanent injury to their spine, but have surprisingly little pain — even none at all in some cases!
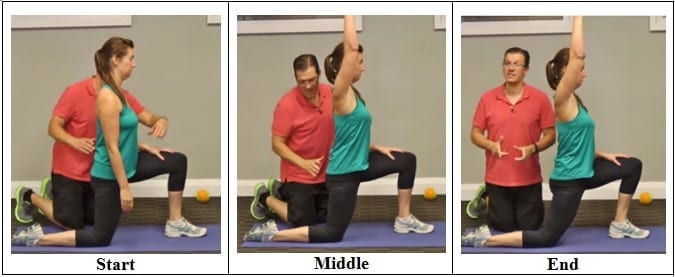
Brace your core and bend your knees to lower down into a split squat. Your left knee should ideally form a 90-degree angle so that your thigh is parallel to the ground, and your right knee is hovering above the floor. (Quick position check: your left foot should be stepped out far enough that you can do this without letting your left knee go past your left toes—if you can't, hop your left foot out a bit farther away from the bench.)
True numbness is not just a dead/heavy feeling (which is common, and caused even by minor muscular dysfunction in the area), but a significant or complete lack of sensitivity to touch. You have true numbness when you have patches of skin where you cannot feel light touch. Such areas might still be sensitive to pressure: you could feel a poke, but as if it was through a layer of rubber. Most people have experienced true numbness at the dentist. BACK TO TEXT
Veritas Health publishes original and accessible health related content written by more than 100 physician authors and peer-reviewed by a 16 member Medical Advisory Board. The Veritas Health platform comprising of Spine-health.com, Arthritis-health.com, Sports-health.com, and Pain-health.com, provides comprehensive information on back pain, arthritis, sports injuries, and chronic pain conditions. For more information visit Veritashealth.com.
Epidural injections of steroid drugs are frequently used to treat sciatica, despite limited evidence for their effectiveness. Moreover, these treatments are based on the assumption that reducing local inflammation in the vertebral column will relieve pain, but an association between structural abnormalities, inflammation, and sciatica symptoms has not been clearly demonstrated. NINDS-funded researchers are using a new imaging technique that can detect inflammation to better understand what causes chronic sciatica pain and to provide evidence to inform treatment selection. 
^ Jump up to: a b c d e f g Hughes SP, Freemont AJ, Hukins DW, McGregor AH, Roberts S (October 2012). "The pathogenesis of degeneration of the intervertebral disc and emerging therapies in the management of back pain" (PDF). J Bone Joint Surg Br. 94 (10): 1298–304. doi:10.1302/0301-620X.94B10.28986. PMID 23015552. Archived from the original (PDF) on 4 October 2013. Retrieved 25 June 2013.

Traction involves the use of weights and pulleys to apply constant or intermittent force to gradually “pull” the skeletal structure into better alignment. Some people experience pain relief while in traction, but that relief is usually temporary. Once traction is released the back pain tends to return. There is no evidence that traction provides any longterm benefits for people with low back pain.

Stop focusing on a specific diagnosis. Up to 85% of low back pain can be classified as "non-specific." This means that the origin of your pain cannot be localized to one specific structure or problem. While common diagnostic tests for low back pain can show the bones, discs, and joints with great detail, no test can tell the exact cause of your pain with 100% accuracy.

But how can you tell? It can be tricky. This is a concise, readable guide to symptoms that need better-safe-than-sorry investigation with your doctor. (It’s basically just a plain English version of clinical guidelines for doctors.9) In other words, this article explains the difference between “dangerous” and “just painful” as clearly as possible. Tables, checklists, and examples ahead.

The AANS does not endorse any treatments, procedures, products or physicians referenced in these patient fact sheets. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific neurosurgical advice or assistance should consult his or her neurosurgeon, or locate one in your area through the AANS’ Find a Board-certified Neurosurgeon” online tool.
If back pain doesn't go away in three months, there's evidence that yoga can help. In one study, people who took 12 weeks of yoga classes had fewer symptoms of low back pain than people who were given a book about care for back pain. The benefits lasted several months after the classes were finished. The study suggests conventional stretching also works just as well. Make sure your instructor is experienced at teaching people with back pain and will modify postures for you as needed.
The story of actor Andy Whitfield is a disturbing and educational example of a case that met these conditions — for sure the first two, and probably the third as well if we knew the details. Whitfield was the star of the hit TV show Spartacus (which is worthwhile, but rated very, very R17). The first sign of the cancer that killed him in 2011 was steadily worsening back pain. It’s always hard to diagnose a cancer that starts this way, but Whitfield was in the middle of intense physical training to look the part of history’s most famous gladiator. Back pain didn’t seem unusual at first, and some other symptoms may have been obscured. Weight loss could have even seemed like a training victory at first! It was many long months before he was diagnosed — not until the back pain was severe and constant. A scan finally revealed a large tumour pressing against his spine.
Quick anatomy lesson. When we talk about the hips, we're talking about any muscle that crosses over the hip joint, says Laura Miranda D.P.T., M.S.P.T., C.S.C.S., a New York City-based trainer and creator of the Pursuit training program. Which, there are many, including all of the glute muscles, the hamstrings, the inner thigh muscles, and the psoas muscles (deep core muscles that attach your pelvis to your spine). Each of these muscles has some specific roles, but overall, the hip muscles stabilize your pelvis and thighbone as you move. They also allow you to bend at the hips, lift your legs out to the side (abduct), and bring your legs back in toward one another (adduct). Basically, they do a lot, and when they're weak or tight or otherwise not working in an optimal way, you can not only end up with cranky hips, but other body parts may overcompensate and take on too much work—leaving you with other, seemingly unrelated, issues, like knee pain.
These are really great tips. Just to imform my friends here, my cousin also gave me this link about some other techniches you can use. You have to know exactly what is going on in your body you know. the product is called Panifix, or "Unlock your hip flexor" which Gives You A Practical, Easy-to-follow Program You Can Use To Instantly Release Your Hip Flexors For More Strength, Better Health And All Day Energy. Proven Swipes And Creatives Here:https://tinyurl.com/yd6nbzfh
Bridge: Still lying on your back with your feet flat on floor, lift your hips and torso off the floor into a bridge. Then interlace your hands underneath your hips and press your shoulders and upper arms into the floor, lifting your hips higher. Hold for 10 seconds. Lower yourself slowly back down, rolling down from the top of your spine to your tailbone. Repeat three times.

Doing the bridge exercise in the morning gets your muscles working, activated, and engaged and will help support you the rest of the day, says Humphrey. Lie on your back with your legs bent and your feet flat on the floor, hip-width apart. Press down through your ankles and raise your buttocks off the floor while you tighten your abdominal muscles. Keep your knees aligned with your ankles and aim for a straight line from knees to shoulders, being sure not to arch your back; hold this position for three to five seconds and then slowly lower your buttocks back to the floor. Start with one set of 10 and build up to two or three sets.

Stop listening to other people’s horror stories. You know the scenario: You are bent over in obvious pain, waiting to see the doctor, and the person next to you tells you a 10-minute tale of how their Uncle Gordon had low back pain that required injections and surgery. But the pain still didn’t go away. Stop listening to these terrible stories. Most low back pain is short-lived and can be managed quite effectively with exercise and postural correction. Of course, some low back conditions are serious and require surgery, but that is a conversation you should have with your doctor, not the guy in the waiting room.

Coccydynia is an inflammation of the bony area (tailbone or coccyx) located between the buttocks. Coccydynia is associated with pain and tenderness at the tip of the tailbone between the buttocks. Pain is often worsened by sitting. There are many causes of tailbone pain that can mimic coccydynia including: fracture, pilonidal cysts, infection, and sciatica. Treatment methods include medication and rest.
Athletes are at greater risk of sustaining a lumber spine injury due to physical activity. Whether the sport is skiing, basketball, football, gymnastics, soccer, running, golf, or tennis-the spine undergoes a lot of stress, absorption of pressure, twisting, turning, and even bodily impact. This strenuous activity puts stress on the back that can cause injury to even the finest and most fit athletes.
Hip pain is a common symptom experienced by many people. This condition can range from mild discomfort to severe pain that limits activities of daily living or functional mobility. Hip pain may prevent you from enjoying your normal work and recreational activities. When you visit a PT for hip pain, he or she will likely investigate the cause of your pain to help treat it properly.
Apply the above concept to your hips. When you sit, your hips are in a "flexed" position. Therefore, the muscles that flex your hips are in a shortened state. You probably spend at least a third of your day sitting down. Think about how much time those hip flexor muscles stay shortened. A lot. Over time, they become tighter and tighter until you look like the old man in the picture. So unless you want to look like that, perform the stretches shown below.
Icing a joint that’s inflamed because of arthritis or bursitis can lower inflammation and help with hip pain. “If it’s very painful, I sometimes tell patients to ice four or five times daily for about 10 to 15 minutes,” says Amy Humphrey, DPT, a physical therapist at Body Dynamics, Inc. in Arlington, Va. Use an ice pack, wrap a towel around it, and put it where you feel the pain.
A complete medical history and physical exam can usually identify any serious conditions that may be causing the pain. During the exam, a health care provider will ask about the onset, site, and severity of the pain; duration of symptoms and any limitations in movement; and history of previous episodes or any health conditions that might be related to the pain. Along with a thorough back examination, neurologic tests are conducted to determine the cause of pain and appropriate treatment. The cause of chronic lower back pain is often difficult to determine even after a thorough examination.
How to: Stand tall, feet slightly wider than shoulder-width apart, toes pointed out at 45-degree angles (a). Keep your back straight, knees over toes and your weight in the heels of your feet (b). Engage your glutes and thighs as you lower into a deep squat until thighs parallel to the ground (or as close as you can get them) (c). Powering through your heels, push up to return to starting position (d). Repeat.
Or anything else. Pain is a poor indicator, period! The human nervous system is really terrible about this: it routinely produces false alarms, and alarms that are much too loud. See Pain is Weird: Pain science reveals a volatile, misleading sensation that is often more than just a symptom, and sometimes worse than whatever started it. BACK TO TEXT